Acute occlusion of the left main (LM) coronary artery leading to cardiogenic shock, so-called the Left Main Shock syndrome (LMSS), is an extremely dangerous lifethreatening conditions.1 Despite successful revascularization, the mortality rates of LMSS remain high, in the ranges of 33-94%.2-4 In Thailand, the prevalence and outcome of this lethal condition is still underreported, thus we disscuss below two LMSS cases that survived emergent coronary angioplasty but who displayed different manifestation and thus altered our treatment decisions.
A 78-year-old lady, had known history of hypertension, presented to out patient department in October 1995 with persistent chest discomfort since several hours. Electrocardiogram (ECG) showed sinus tachycardia with ST segment elevation (STE) in leads I, aVL,V1-5 which was suggestive of an acute ST segment elevation myocardial infarction (STEMI) involving antero-apical and lateral wall. She suddenly became hypotensive with blood pressure (BP) of 80/40 mmHg and was urgently transferred to catheterization room. It was evident that she had frank pulmonary edema, cardiogenic shock (CS) complicating acute myocardial infarction (AMI). Heparin 5,000 unit and aspirin were administered. After arriving, her BP continuously declined and became un-measurable. Intubation and intra-aortic balloon (IABP) counter-pulsation were performed along with temporary pacing for treatment of intermittent bradycardia. The echocardiogram showed severe hypokinesia of anterior-apical and lateral wall with estimated left ventricular (LV) ejection fraction (EF) of below 40%.
Subsequently she developed several episodes of ventricular fibrillation (VF) arrest, on and off, requiring intermittent cardioversion and cardiopulmonary resuscitation. The coronary angiogram performed during cardiac massage showed a subtotal stenosis of the mid left main (LM) body (Figure 1) resulting in diminished flow downstream (TIMI flow grade 2) to the left anterior descending (LAD) and circumflex (Cx) arteries. The dominant right coronary artery (RCA) was unobstructed but did not provide any significant supply to the left arteries (Figure 1B). Owing to her extremely unstable condition, we decided to perform direct balloon angioplasty of the LM.
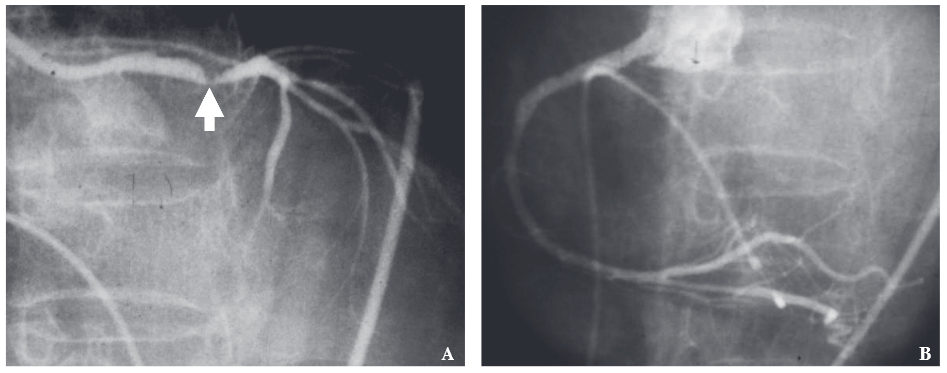
Figure 1: Coronary angiogram showed intra-luminal thrombus in the body of the left main coronary artery (arrow) causing a subtotal luminal stenosis (A). An unobstructed right coronary is shown in B.
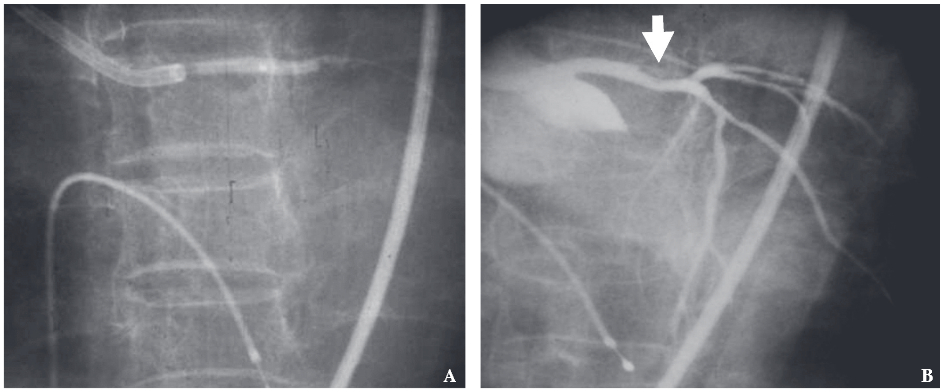
Figure 2: Balloon dilatation (2.0/20) was performed during cardiopulmonary resuscitation (A) an resulted in re-establishedcoronary flow with residual stenosis of less than 20% (open arrow in B).
Balloon dilatation (2.0/20 balloon) was emergently performed during intermittent cardiac massage. After multiple short inflations and episodes of ventriculer fibrillation (VF) and bradycardia, the flow was finally re-established and she became more stable. Final angiogram (Figure 2B) showed a residual stenosis of less than 20% with no intimal dissection and the flow was normal. It should be noted that in 1995, stent were still not available so we accepted the result.
The patient slowly recovered from heart failure and pneumonia but survived. After spending weeks in coronary care unit (CCU), she was transferred to another hospital where her daughter worked as and was discharged home two months later. In 1998, she fractured a hip and was referred for pre-operative evaluation. The coronary angiogram showed a patent left main with no residual stenosis (Figure 4). There was no new lesion in the rest of her arteries. Owing to severe osteoporosis, the orthopedist decided to treat her conservatively and she is lost to follow up since then. This case represented the first primary coronary intervention for AMI in Bhumibol Adulyadej and in our country as well.
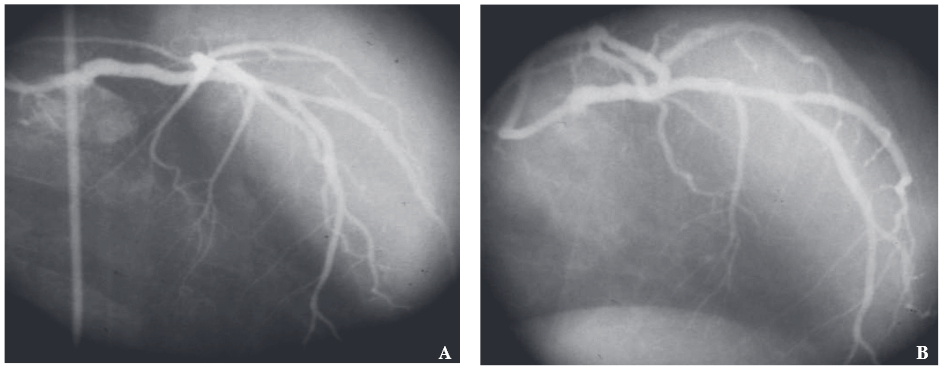
Figure 3: Coronary angiogram performed 2.5 years later in 1998 and showed a smooth lumen of the left main trunk with no re-stenosis.
A 60-year-old man, cigarette smoker, developed chest tightness while riding a motorcycle over the period of one hour. He presented to emergency room (ER) in July 2005 with BP of 71/43 mmHg, HR of 75/min. The 1st ECG showed sinus rhythm with 3-5 mm ST depression (STD) in leads II, I, aVL and V2-V6 in conjunction with > 1mm STE in lead aVR and V1 (Figure 4). Echocardiogram delineated akinetic lateral wall, hypokinesia of anterior wall with the ejection fraction (EF) of less than 40%. Physical and laboratory findings were consisting with left heart failure and CS complicating the non-STEMI. Oral aspirin, clopidogrel, intravenous heparin and Tirofiban were given at ER before he was taken to the lab. On arrival, he still had 10/10 chest pain, BP was 87/54 mmHg, HR was 93/min in sinus rhythm. Right heart catheterization showed an elevated pulmonary capillary wedge pressure (PCWP) of 33 mmHg and intra-aortic balloon pump (IABP) was placed. Owing to low oxygen saturation, intubation with ventilatory support was performed.
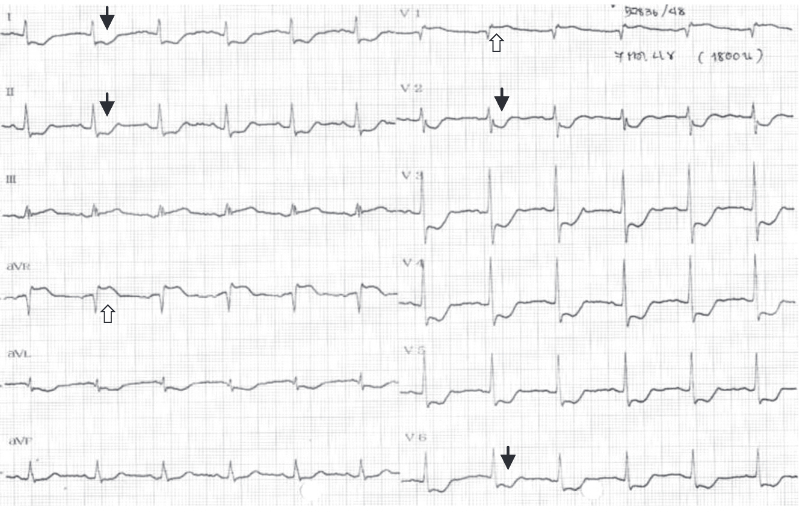
Figure 4: The 1st ECG of case report 2 showed diffuse ST segment depression in leads I, aVL, II, V2-V6 (black arrow) and > 1mm ST elevation in leads aVR and V1 (white arrow). Early transition (tall R in V2) suggested posterior wall extension.
Coronary angiogram revealed a totally occluded LM artery at distal bifurcation with no antegrade flow (TIMI flow grade 0). An unobstructed RCA provided major collateral supply to the left coronary arteries (Figure 5). Cardiothoracic surgery team were consulted but were not available until for the next 6 hours. Despite IABP support, he was still hypotensive and progressively deteriorating so we decided to open the occluded LM artery.
Attempts to pass the guide wire were successful only into the distal Cx but not into the LAD artery. After the 1st balloon inflation at mid-distal LM, he had PVCs and short run of ventricular tachycardia (VT), see Figure 6, but the flow to Cx artery was improved. Shortly, he became hypotensive again with systolic BP of 70 mmHg and junctional rhythm with wide QRS complex. To secure the flow in LM artery, a stent was then deployed at mid-distal LM trunk, which restored the flow and blood pressure. He was pain free and clinically stable. Post percutaneous transluminal coronary angioplasty (PTCA), ECG showed sinus rhythm with normalized ST-T changes (Figure 7).
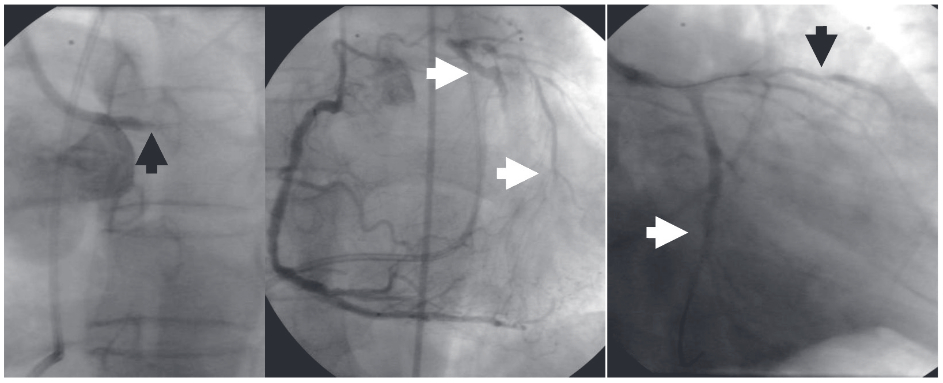
Figure 5: Showed a totally occluded distal LM artery (black arrow, left) and unobstructed right coronary artery (middle) that provided a major collateral supply to distal part of the left coronary artery (white arrows). After balloon dilatation, the flow improved to Cx and proximal LAD/diagonal arteries (black arrow, right) but we could not pass the wire across an obstructed LAD artery.
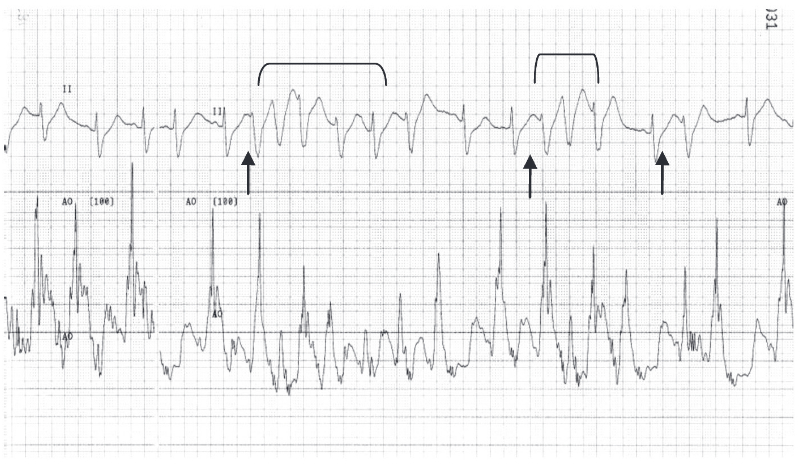
Figure 6: Upper tracing showed frequent short coupling premapure vemtricular complexes (PVCs) (black arrow) induced non-sustained VT (in bracket) during and after balloon dilatations resulted in transient hypotension (arterial pressure 50-60 mmHg in lower tracing)
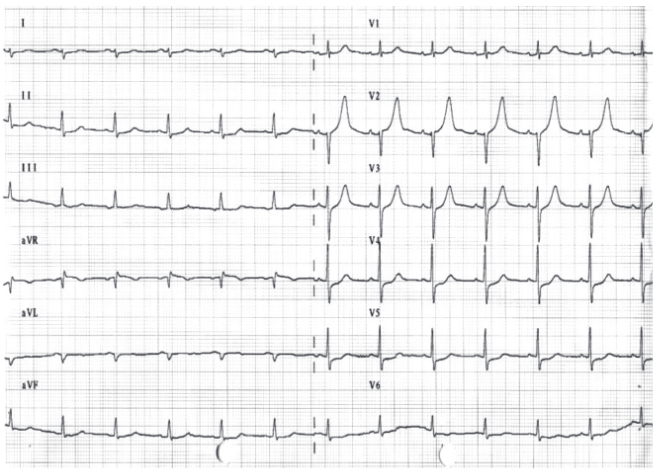
Figure 7: ECG after PTCA showed improvement of ST depression in all leads and lesser degree of ST elevation in lead aVR. Tall R in V1, Q in V2 and tall T in V1-3 were also noted.
For better long-term result, the CVT team was re-notified and he underwent successful coronary bypass grafting, with SVG to LAD and to Cx arteries, on the next day. After three days, IABP and endotracheal tube were removed. He was transferred to regular ward the following week and was discharged on the 22nd day. He is still alives at present.
1. Prevalence of LMSS
Both of our cases displayed a serious AMI complication, CS (a state of systemic tissue hypo-perfusion due to pumping failure in the presence of adequate volume5), resulted from acute total (case report 2) and sub-total (case report 1) LM occlusion. Generally, CS is uncommon, occurred in 5-8% of AMI but the mortality is high, over 50%, in the setting of STE-MI.6 The prevalence of AMI caused by severe (luminal narrowing>75%) stenosis of an unprotected (de novo) left main artery (AMI-LM) is even rarer, varied from 2.4-5%.1, 2 Since the LM artery mostly supplied blood to the LV, abrupt thrombotic occlusion shortly produced the states of pulmonary edema, CS and sudden death. Although the AMI-LM had been formerly reported,7, 8 the term LMSS was introduced in 19931 to describe a highly fatal CS that occurred in 44% of patients suffering from antero-lateral MI, like case report 1. In Quigley and colleagues’ report, the mortality was very high, despite treatment, up to 94%.1 Subsequent studies showed a reduction of LMSS mortality from 76% with combine revascularization3 to 33% with direct coronary stenting.4 Therefore, early detection and treatment is essential to preserve the life of patients with this condition.
2. Clinical & ECG recognition
Victims of LMSS victims tend to manifested in the same fashion, having chest pain, shortly afterwards developed pulmonary edema and later CS within few hours2, 9-11 and so did our cases. In one report, 16% of AMI-LM presented with unstable angina.12 In a large retrospective study of 131 patients suffering from acute coronary syndrome (ACS) due to de novo LM stenosis,13 half of them presented with STE-AMI or CS (49.6%) and the rest (51.3%) had unstable angina/non-STEMI, like case report 2. Most of the victims were men, 73-84%2, 13 and had the mean age of 67 (46-89) years.2 Our cases shared the same age range (78 and 60 years) and had occurrences of life threatening ventricular arrhythmias. Patient 1 had frequent VF before angiogram and patient 2 had non-sustained VT during coronary intervention. In 18 AMI-LM cases reported by Yip et al, 94% had pulmonary edema and 33% died from malignant ventricular arrhythmias.4
ECG recognition remained a primary step in diagnosing LMSS. Our first patient had diffuse ST segment elevation (STE) in anterior and lateral wall (leads I, aVL, V1-5, ECG was not available) associated with STD in inferior leads, which was found in majority of the LMSS cases.1, 9, 10, 13 A less common pattern, precordial STD as shown in case report 2, was found in 21.8% among 32 AMI-LM cases.14 In addition, the aVR lead (representing the basal septal area) displayed STE (> 0.05 mV) which was quite characteristic in AMI-LM cases.14, 15 The degree of STE in aVR, that was either equal or higher than those of V1 lead, reliably distinguished the AMI-LM from AMI secondary to proximal LAD artery occlusion, with the sensitivity, specificity and predictive value of 81, 80 and 81% respectively.14 Recently, body surface mapping ECG had been shown superior to 12-lead ECG in detecting AMI-LM, with the sensitivity of 88% and specificity of 83%.16
3. Prognostic indicators
Mortality predictor are crucial in LMSS since they identified high fatality candidates. The presence of shock, as defining LMSS, by itself already carried a high mortality, from 33-76% despite treatment.2, 3, 12, 13, 17-19 In the SALVage study of 131 AMI-LM cases, the CS/STEMI group had higher mortality than those of non-CS, NSTEMI group, 44% vs. 6%, p < 0.001.13 By univariate analysis, the occurrence of VT/VF, as found in case report 1, was the most powerful mortality predictor and significantly reduced the short term survival.3 By angiographic parameters, the pre-intervention antegrade flow (TIMI flow grade ≥ 2),13, 19 the incomplete stenosis of LM,2, 13, 19 the presence of collateral supply 2, 11, 17, 18 and the right dominant coronary system 2, 12, 17 had been found to be good prognostic indicators in LMSS cases. Those parameters attenuated the degree of myocardial ischemia and clearly explained the survival causes of our two cases. In case report 1, the LM artery was still patent with TIMI flow grade 2 and she had a large unobstructed RCA. In case report 2, the well developed collateral supply was obtained from a dominant RCA.
4. Choices of revascularization
Both percutaneous coronary intervention 2, 4, 12, 19, 20 and bypass surgery 3, 10, 11, 17, 18, 21 have been effectively performed but with the high mortality in comparison when those procedures are used electively. Currently, there is still no randomization study which compares between these two reperfusion strategies in AMI-LM22 or CS from multi-vessel coronary artery disease.23 Although CABG remains the gold standard for stable LM patients, the guideline recommendations for treating AMI-LM or CS remain unclear.22 The recent ECC/ EACTS myocardial revascularization guidelines in 2010 still recommended CABG surgery as a class IA for LM disease but spared the isolated ostium or shaft LM lesion as class IIa(B).24 This also based on the fact that 80% of LM disease either involved distal bifurcation or there are other coronary lesions present which would benefit from CABG surgery.24 The current ACCF/AHA/SCAI 2011 guideline for percutaneous coronary intervention (PCI) recommended the same thing, CABG for LM disease (class 1A), and class IIa(B) for PCI of LM to improve survival in unstable angina/NSTEMI patients who are not candidates for CABG and in patients with acute STEMI from LM who have distal flow < TIMI 3 under the condition that PCI can be performed more rapidly and safely than CABG.25
Practically, the choice of revascularization solely depends on the patient’s condition (CS or stable), the site of the lesion (ostial, body or distal LM), concomitant lesions in other arteries, experience of operator, team and the availability of surgical colleagues. In the ideal situation, if the patient becomes stable after IABP placement, CABG would be a reasonable choice for long term benefit. However, typical LMSS cases are critically ill and died quickly either due to pump failure or ventricular arrhythmias, therefore PCI could be a life saving procedure as was demonstrated in our cases. The 1st patient was dying from her frequent VF and emergent PCI saved her life. The lesion at shaft of LM with no bifurcating disease or other lesions was also suitable for PCI. Without stent, this lesion healed up well after 2.5 years with no restenosis. The second case represented a bridging PCI, which was performed as the patient’s condition deteriorated, in order to stabilize the patient and by the time before surgery. The bifurcating lesion was certainly not ideal for PCI and the result was still suboptimal. Fortunately he had major supply from RCA and became stable after stenting LM. He is still alive at the present time. Nowadays, a thrombus aspiration device would be suitable for removing a clot from an occluded left main artery before placing a stent. These devices have been effective in reducing infarct size, improved myocardial perfusion and 1-year clinical outcome.26, 27
We reported two LMSS cases who survived after life-saving PCI: one with direct balloon dilatation and another with bridging coronary intervention before bypass surgery. Both cases shared the common and rarer features of LMSS and the typical ECG findings. We reviewed clinical recognition and prognostic indicators along with choices for revascularization. We hoped that the details would be beneficial for emergency physicians internist and cardiologist who may face with this lethal LMSS patients some day.