Pulmonary nodules and lesions are common findings since chest x-ray and CT scan have become a screening method for lung cancer.1 Several guidelines on lung malignancy screening have been formulated in order to solve the increasing percentage of this disease worldwide. As a general practice, lung nodules would be followed by clinicians by CT scan monitoring, bronchoscopic methods such as Fiberoptic bronchoscopy (FOB) or endobronchial ultrasound bronchoscopy (EBUS) as well as invasive techniques like transthoracic needle aspiration (TTNA) or surgery (lobectomy).2
CT scan monitoring or watchful waiting carries the risk of late detection of disease progression.2 FOB though less invasive among surgery, could not reach the outer third of the chest and small nodules, providing very low efficiency.3,4 While EBUS has the highest yield among all diagnostic techniques, it does not have the real time guidance and directions that could facilitate the accurate nodule location finding. TTNA and surgery are generally associated with the greatest risk of pneumothorax among all procedures.5
There is an urgent need to identify safe, practical and more accurate ways to diagnose nodules and lesions that are harmless to the patient.
Electromagnetic Navigation Bronchoscopy (ENB) is a cutting edge technology that allows pulmonologists a very precise identification of the target pulmonary nodule by using mechanics similar to a global positioning system (GPS) apparatus. This equips the physician with a direct course towards the target lesion, making it easier to obtain tissue sample from small nodules and attain hard to reach target areas.6,7
This study will describe our experience and illustrate the yield while using ENB in combination with EBUS as a diagnostic tool among patients with suspected lung malignancy.
A retrospective analysis was conducted for 33 patients between November 2014 and November 2015 at the Bangkok Hospital Medical Center. Patient age, gender, race (Asian or non-Asian), smoking history, lung nodule location and final diagnoses were collected. ENB with EBUS under IV sedation among patients with 2 to 108 mm lung nodules with suspected lung malignancy were performed. Yield was determined by attaining final diagnosis from tissue analysis of every patient who underwent the ENB and EBUS procedure. Patients with no definite diagnosis were referred to surgery for further examination. The intraoperative and postoperative complications were recorded.
ENB and EBUS procedure was completed on 33 subjects comprised 67% (22) males and 33% (11) females, aged 37 to 77 with mean of 61 years old. Asian patients represented 29 (88%) cases and Non-Asians were 4 subjects (12%), among them 7 were (21%) smokers, 17 (52%) nonsmokers and 9 (27%) former smokers. 26 cases (79%) were provided with definite diagnosis through the bronchoscopy while 6 (18%) subjects were referred to surgery and 1 (3%) case refused further investigation.
Lung nodules were located in the upper lobe (52%), lower lobe (43%) and middle lobe (5%). Lymph node involvement was present in 33% of the cases.
The diagnoses of the 33 patients were the following: lung cancer: (10) 30%, lung cancer and nontuberculous mycobacteria infection (NTM): (2) 6%, lung cancer and tuberculosis (1) 3%, tuberculosis (5) 15%, nontuberculous mycobacteria infection (NTM): (4) 12%, lung infection/ bronchiectasis: (5) 15%, benign nodules (4) 12%, hamartoma (1) 3%, no definite diagnosis: (1) 3%.
Lung cancer cases (13) were adenocarcinoma: 10, squamous cell carcinoma: 1, gastrointestinal stromal tumor (GIST): 1 and small cell carcinoma: 1.
No complications were recorded on all 33 patients.
Currently, there are different guidelines for lung cancer screening worldwide. Each has their own approach on timely diagnosis, accuracy and treatment options. However, all of them have a common ground which begins with detection of lung nodules and lesions through low-dose chest CT scan. One of the better known successful studies on this is the National Lung Screening Trial (NLST) which found that participants who undergone low-dose CT scan had a 20% lower chance of lung cancer mortality.8
If all lung cancer screenings begin with low-dose CT scans,the quantity of suspicious pulmonary nodules may possibly increase remarkably in the future.9 For each patient found with pulmonary nodule or lesion, clinicians should take into consideration the patient’s status, clinical manifestation, availability of skilled physicians and accessibility of the institution to modern technology.
A large number of suspicious lung nodules are seen on patients who are at high risk for surgery and some of them are too weak to undergo transthoracic needle aspiration.10 Complications such as pneumothorax should be considered prior to performing further investigations.11 Hiraki T et al12 conducted a retrospective study that showed 40% of pneumothorax rate out of >1000 patients who undergone CT-guided lung biopsy, with 11% needing chest tube insertion. The risk of pneumothorax generally increases as the nodule becomes smaller and deeper inside the lung.
Obtaining tissue for the diagnostic purposes should be performed in the least invasive manner for the patient. Baaklini WA et al.4 stated in their study that the sensitivity of fiberoptic bronchoscopy in the diagnosis of endobronchial lung abnormalities was about 90% in major pulmonary airways but only 14% in small and peripheral lung lesions.The examination of lung abnormalities that are not seen through a bronchoscope is very challenging. However, the major benefit of utilizing bronchoscopic approach over surgery or other more invasive technique is fewer risks and complications. One of the modern bronchoscopic tools that have emerged in the 1990’s is the Endobronchial Ultrasound (EBUS). EBUS has proven to be effective worldwide.13 This procedure uses ultrasound waves to confirm the presence of even the smallest nodules, and then use a brush or needle for tissue aspiration. EBUS provides one of the highest yields when it comes to lung nodule investigation,14 however further improvements can be attained if pulmonologists can reach further into the smaller branches of the bronchial tree with the assistance of the electromagnetic navigation system.15
In a study by Eberhardt R. et al,6 the combination of EBUS and ENB has a yield of 88% which is higher compared to using each technique independently, with EBUS having a 69% and ENB a 59% yield. In our research, we were able to achieve a yield of 79% using a combination of EBUS and ENB. This proves that with ENB, the lung abnormalities that the EBUS was unable to reach meant that even the smallest size of lesions or nodules located on the upper lobe and other third of the lung could be reached by the extended working channel of ENB. Furthermore, there were no incidents of any complications such as pneumothorax, bleeding or infection. Although the timing was not recorded for each procedure, the duration of the procedure was not a concern as the integration of EBUS and ENB required minimal additional time.
ENB a wide range of applications such as placement of fiducial markers, brachytherapy catheters or marking of bronchoscopic pleural dye for the surgical removal of lesions. ENB is compatible to use with other instruments such as FOB or EBUS.15 Moreover, ENB can be use independently without the need of fluoroscopy compared to other equipment used in investigation of lung abnormalities.6
ENB is a straightforward navigation system that provides direct visualization to the lung nodule that facilitates accurate tissue biopsy which increases diagnostic yields. As lungscreening programs becomes extensive widespread worldwide internationally, the investigation of lung nodules should be kept minimally invasive especially for the compromised and weak patients. This novel innovative technology can provide precise directions for correct lung tissue diagnosis without causing further harm to the patients.16
ENB is an effective, accurate and a novel method that provides real time navigational guidance toward lung lesions and nodules. This technology allows flexibility that aids biopsy on hard to reach areas attains larger tissue samples and stops bleeding better than conventional bronchoscopy. This instrument complements other bronchoscopic methods such as EBUS that and allows a higher yield compared to using one bronchoscopic method alone. In our study, we were able to obtain a yield of 79% by using the combination of ENB with EBUS.
This is a case of a 44-year-old male, who came for consultation due to moderate hemoptysis for two months. In 2013, he was suggested of tuberculosis (TB) and was prescribed with anti-TB medications for nine months. During follow up check-up in 2014, he was asymptomatic and chest x ray only showed old scar tissue. The following year, chest x ray reported cavitation at right upper lobe. His Acid Fast Bacilli (AFB) was negative on four occasions but hemoptysis persisted. He has no known underlying disease and is a non-smoker.
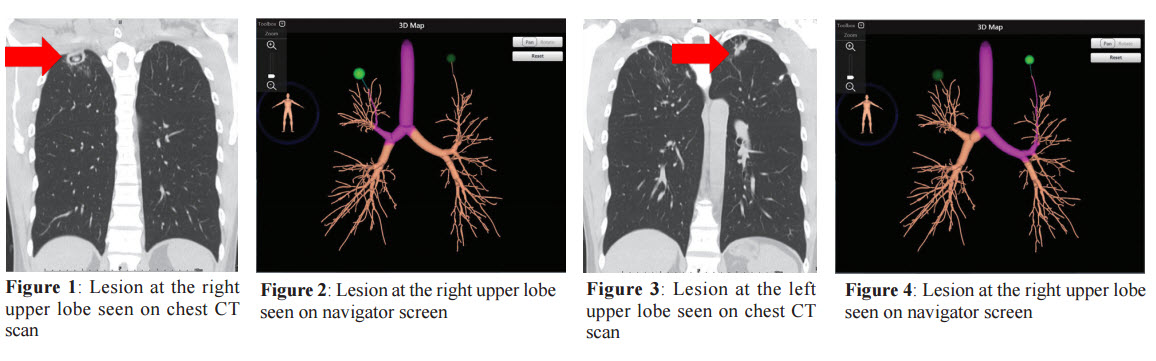
Physical examination revealed cough with bloody secretions, mild dyspnea, chest itchiness and four kilogram weight loss. His vital signs were: temperature: 36.3 OC, pulse rate: 70/min, respiratory rate: 18/min, BP: 138/78, O2 saturation: 97%. Chest CT scan reported that there is a 2.4-cm, smooth thin wall cavitary lesion with associated adjacent centrilobular nodules with tree-in-bud opacities at the apical segment of the right upper lobe. There are several calcified pulmonary nodules at the apical segment of the right upper lobe, and apicoposterior segment of the left upper lobe, fibrocalcific scar at the apicoposterior segment of the left upper lobe as well as several fibroses at both upper lobes. These findings are likely consequence of old granulomatous infection. Blood test for TB, which is Quantiferon TB was negative. Endobronchial Ultrasonogram Guided Sheath (EBUS GS) and Electromagnetic Navigation Bronchoscopy (ENB) under Fluoroscopy were advised for further assessment and evaluation. There were two lesions found during the procedure. With the guidance provided by the navigator, tissue specimens were obtained from right and left upper lobes. No complications were noted post-biopsy.