Diabetes mellitus is the most important global health problem burden. The prevalence rate of diabetes has continued to increase from 371 million people worldwide in 2013 to 415 million persons; and 5 million people died from diabetes in 2015. It is estimated that approximately 642 million people or one in every ten persons will have diabetes by 2040.1 Thailand also faces diabetes problems with over 4 million cases of the disease in 2015 and an expected increase to 5.1 million cases by 2035. The mortality rate of persons with diabetes has also raised from 20,654 cases in 2014 to 75,994 cases in 2015.2 These burdens are the results of uncontrolled blood sugar.
Poor glycemic control over a long period of time in persons with T2DM is significantly able to damage all nerves and blood vessels, especially in vital organs, such as cardiovascular disease, diabetes nephropathy, diabetes retinopathy, and diabetes neuropathy.1These adverse consequences lead to a high cost of care and higher hospitalization rates directly impacting on family and socioeconomic status.3 So, persons with uncontrolled T2DM have to continuously control their HbA1c level within the normal range not only by taking medicines, but also modifying lifestyle performance such as diet control and regular exercise.4,5 However, approximately 62% of people with uncontrolled diabetes were not able to integrate healthy diet behavior into their lifestyle practice caused by a lack of self-control resulting in adverse consequences such as weight gain and higher blood sugar levels.6 Hence, burning more calories from dietary intake through regular exercise seems to be a beneficial way for persons with uncontrolled T2DM.
An exercise being easy, safe, and convenient to perform without any equipment is an arm swing exercise (ASE) which is a Traditional Chinese Medicine practice classified as a mild-moderate intensity exercise utilizing 45-60 percentage of maximal heart rate.8 The ASE integrated with posture and meditation will stimulate blood circulation resulting in blushing face, sweating and stretching as well as relaxed tendons and muscles through the body in order to relieve illness especially chronic diseases such as diabetes.9,10 Moreover, exercise exerts as an insulin-like effect helping to increase glucose uptake in the skeletal muscle by translocation of glucose transporter 4 (GLUT4) from an intracellular location to the plasma membrane leading to improved insulin sensitivity and reduced insulin resistance.11 Likewise, performing regular ASE can increase insulin concentration and insulin sensitivity leading to decreased HbA1c level.10,12 Moreover, ASE is able to enhance fat oxidation leading to a decrease of total fat mass changing to skeletal muscle.11,13
However, there is still controversy in studies regarding ASE and its outcomes such as reduced body mass index (BMI), waist circumference or visceral fat in persons with T2DM. Most of previous ASE intervention studies emphasized one group pre-posttest design or the participants served as the control group before being in the experimental group and had different frequency and duration of the ASE intervention having a range from approximately 20-30 minutes a day 3-7 days a week for 6-8 weeks.8,10,12,14 Therefore, this experimental study increases frequency and duration of ASE program to perform ASE for 30 minutes a day, 5 times a week, 12 weeks in order to accomplish health outcomes in persons with uncontrolled T2DM.
Besides, the number of persons with diabetes in Suphanburi province is still high. In 2014, there were only 4,540 persons who were able to control blood sugar level within normal range in a total of 10,918 persons in the province. It is clear that approximately 59% of all diabetes cases cannot control their blood sugar level within the normal range.15 Although, Ban Phai Rong Wua Sub-district Health Promoting Hospital and Ban Long Thong Sub-district Health Promoting Hospital in Songphinong District take care of persons with diabetes following Diabetes Clinical Practice Guideline of Ministry of Public Health guidelines, numbers of diabetes patients have gradually increased from 341 in 2015 to 359 in 2016 and from 223 to 242, respectively. Indeed, this problem should be solved by using an effective method.
Unfortunately, some studies reported that 47% of all persons with uncontrolled diabetes cannot continuously exercise following recommendations due to various reasons particularly lack of self-efficacy.6,7 Thus, it is necessary to promote perceived self-efficacy for exercise in persons with diabetes to effectively increase in motivation, inspiration, and confidence to continuously perform exercise. Following Bandura’s concept,16 there are four resources to enhance perceived self-efficacy for health behavior modification including: mastery experience, vicarious experience, verbal persuasion and physiological and effective states.16 If people with uncontrolled diabetes perceive their ability to perform ASE and expect regular ASE to be a better way to achieve glycemic control and prevent complications, they will perform ASE regularly. So, the ASE Program integrating self-efficacy perception in this study involved motivating activities as shown in Figure 1.
Therefore, the present study was aimed at determining the effects of the ASE Program on blood sugar levels (HbA1c), BMI, waist circumference, visceral fat, skeletal muscle, and perceived self-efficacy for exercise in persons with uncontrolled T2DM. The findings could help to develop the ASE program in persons with uncontrolled T2DM contexts resulting in preventing diabetes complications and improving quality of life.
An experimental research design of two-group pretestposttest design was used for this study. The population was persons with uncontrolled T2DM at Ban PhaiRong Wua and Ban Long Thong Sub-district Health Promoting Hospital, Suphanburi Province, Thailand during December of 2016 to April of 2017.
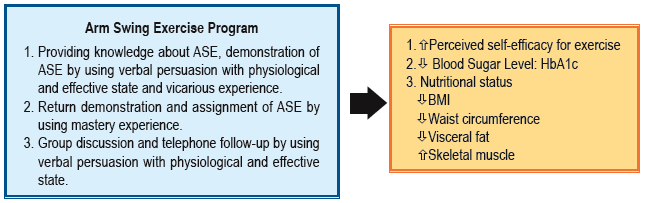
Figure 1: Conceptual framework on the effects of the ASE program on blood sugar level, nutritional status and perceived self-efficacy for exercise in persons with uncontrolled T2DM.
The inclusion criteria:
The exclusion criteria: Admitted in the hospital, adjusted drug, or practicing ASE less than 80 %.
The sample size was determined based on Power Analysis using G*Power software17 sufficient for t-test statistics with statistical power at 0.80, p-value at 0.05, effect size at 0.69 according to a previous study8,10,12,14,18 obtaining a sample of 27 participants per group. Approximately 10% was added, obtaining the final sample of 30 participants per group.
A simple random sampling was used to assign two health promoting hospitals into the experimental and control groups. The researcher also designated the participants who met all inclusion criteria. Then the potential participants who were willing to participate were randomly selected without replacement until the desirable sample size was obtained for each group. However, there was one participant in each group who were later excluded during the study.
Research Instruments
The instruments used in this study were divided into two parts as follows:
Part 1: Instrument for experiment; ASE was adapted from Sangthong Terathongkum and colleagues19 by a little bending of the knees at the third ASE performance. This program included knowledge, demonstration and return demonstration of ASE, ASE assignment at least 30 minutes a day 5 times a week for 12 weeks at home, telephone follow-up approximately 20 minutes/time at week 2,3,5,6,7,9,10, and 11 and group discussion for 60 minutes at week 4, 8, and 12. Three experts including a physician, a nurse instructor, and an advanced practice nurse validated the content of the program. The content validity index (CVI) of this program is equal to 1.
Part 2: Instruments for data collection; Instruments for data collection were divided into four domains as follow:
Data collection
After participants signed the informed consent form, data was collected by the researcher in the following procedures. At baseline assessment in the first week, all participants were asked to provide the demographic characteristics and the perceived self-efficacy for exercise. The participants were also assessed for HbA1c, BMI, waist circumference, visceral fat and skeletal muscle. Then, the participants in the experimental group received the ASE program included knowledge and demonstration of ASE by using verbal persuasion with physiological and effective state and vicarious experience. Return demonstration and ASE assignment at least 30 minutes a day 5 times a week at home were integrated to promote mastery experience. Telephone follow-up approximately 20 minutes/time at week 2,3,5,6,7,9,10, and 11 and group discussion for 60 minutes at week 4,8,12 using verbal persuasion with physiological and effective state in order to motivate self-efficacy for exercise. Whereas, the control group received routine nursing care following “seven colors of ping-pong” representing diabetes condition management based on individual blood sugar level. After immediately finishing the program, all remaining participants in both groups were measured for perceived self-efficacy for exercise, HbA1c, BMI, waist circumference, visceral fat and skeletal muscle to evaluate actual effects.
Data analysis
A statistical computer software program was used to analyze data. Descriptive statistics was used to explain the demographic data. Baseline of demographic data used the Chi-square or Fisher’s exact test for comparison of categorical variables, while Student’s t-test was used for normal distribution data and achieved all assumptions required. Then, comparisons of the average blood sugar level, nutritional status and perceived self-efficacy for exercise within the group was undertaken using Paired t-test and comparison between groups was achieved using Analysis of Covariance (ANCOVA).
Ethical considerations
This study was approved by the Institutional Review Board (IRB), Faculty of Medicine Ramathibodi Hospital, Mahidol University, Thailand (ID 10-59-26).
Sixty persons with uncontrolled T2DM were randomly divided into two groups with 30 participants in each group: an experimental group from Ban Phai Rong Wua Sub-district Health Promoting Hospital and a control group from Ban Long Thong Sub-district Health Promoting Hospital. Two participants withdrew from the study because of referral to district hospital for adjusted anti-hyperglycemic drug at the fourth week and moved to another province at the twelfth week. Thus, 58 participants taking unchangeable medicine remained in the study including 29 participants each group.
The findings revealed that most of the experimental group and control group were females (69% and 82.8%, respectively). Average age of the experimental group and control group was 60.24 years (SD = 9.28) and 62.59 years (SD = 11.17). Most samples were married (75.9 % and 62.1 %) and the highest educational attainment was elementary level (86.2% and 89.7 %). Most of the experimental group was employed in agriculture (34.5%) while the control group was mostly made up of employees (44.8%). They had a mean duration of diabetes equal to 7.28 years (SD = 5.19) and 7.41 years (SD = 4.53), respectively. Both groups used diabetic medication (96.6%). The experimental group controlled HbA1c level by taking oral anti-hyperglycemic drug such as Metformin and Glipizide (51.7%) whereas the control group controlled it by taking only Metformin (55.2%). Hypertension was a co-morbidity in the experimental group with 31.0% and the control group with 37.9%. All independent variables in demographic data were not significantly different in both groups except occupation tested by Chi-square, Fisher’s exact test, or Student t-test depending on scales of each variable.
Before the ASE Program, only HbA1c and waist circumference were different between groups as shown in Table 1. Nobody had hypoglycemia during the Program. After receiving the Program, the experimental group had significantly lower mean of HbA1c level (t = 3.04, p < 0.01), higher mean of skeletal muscle (t = -2.32, p < 0.05) and perceived self-efficacy for exercise (t = -11.53, p < 0.001) when compared with before receiving the Program as shown in Table 2. Using pretest as a covariate in ANCOVA, the experimental group had significantly lower waist circumference (F = 8.66, p < 0.01) and higher perceived self-efficacy for exercise (F = 303.78, p < 0.001) than the control group as shown in Table 3.
Table 1: Comparison of average HbA1c, body mass index (BMI), waist circumference, visceral fat, skeletal muscle and perceived self-efficacy for exercise of the experimental group and the control group before receiving the Arm Swing Exercise Program using Descriptive statistics and Student’s t-test. (n = 58)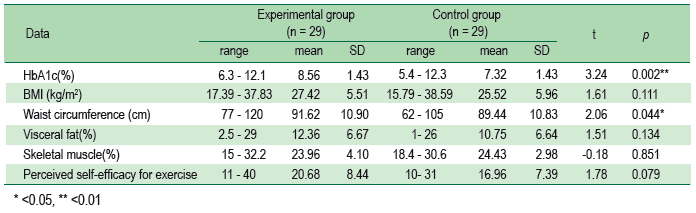
Table 2: Comparison of average HbA1c, BMI, waist circumference, visceral fat, skeletal muscle, and perceived self-efficacy for exercise after receiving the Arm Swing Exercise Program in the experimental group by using Paired t-test (n = 29)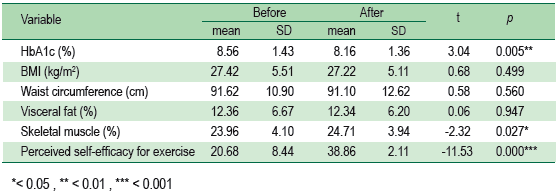
Table 3: Comparison of average HbA1c, BMI, waist circumference, visceral fat, skeletal muscle and perceived self-efficacy for exercise after receiving the Arm Swing Exercise Program between control group and experimental group by using ANCOVA (n = 58)
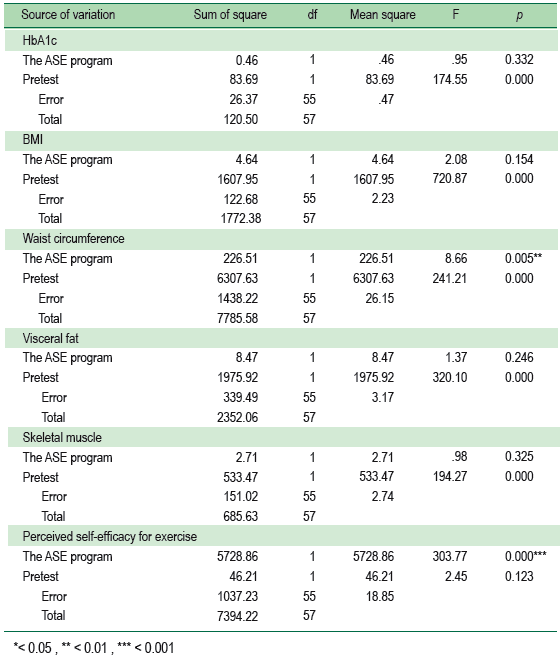
The experimental group had significantly lower HbA1c, higher mean of skeletal muscle and perceived self-efficacy for exercise when compared to before receiving the program. Means of waist circumference and perceived self-efficacy for exercise of the experimental group were significantly better than the control group. These resulted from participants receiving the ASE Program integrating with Bandura’s Self-efficacy theory using four important resources to be mediator.16,19 The ASE program helped to inspire all participants in the experiment group to continually perform ASE using many methods such as group discussion and telephone follow-up for solving exercise problems by providing verbal persuasion with physiological and effective state. Thus, the ASE is able to enhance fat oxidation assisted to reduce visceral fat through skeletal muscle12 resulting in decreased waist circumference assisting to improve insulin sensitivity, reduce insulin resistance and increase glucose uptake resulting in a decreased HbA1c level.10,12 These results were similar to some studies which found benefits of ASE in significantly reduced FBS (p < 0.05) 18 when participants performed ASE 30 minutes a day, every day for 6 weeks or at least 20 minutes a day, 3 times a week for 12 weeks.14 Few studies also revealed that the ASE Program at approximately 30 minutes a day, 3 days a week for 8 weeks significantly reduced HbA1c (p < 0.05).8,10,12 However, those previous studies did not show the effects of ASE on reduction of waist circumference.8,10,12 These ineffective results may be caused by insufficient use of energy from ASE. Therefore, it is obvious that performing ASE for 5 times a week for 12 weeks is an adequate use of energy for reducing waist circumference among persons with diabetes as shown in this study.
Unfortunately, the experimental group had no significantly lower mean of BMI, waist circumference, and visceral fat than before receiving the program. These might result from lower metabolic rate of elder participants.20 Therefore, energy use from the ASE might be less than their energy intake. These results were like previous studies.8,10,12 Thus, the ASE Program should integrate dietary control to improve HbA1c and nutritional status in persons with uncontrolled T2DM.
Besides, the significant outcomes between groups in this study were composed of waist circumference and perceive self-efficacy for exercise being the effect size calculating by ANCOVA formula equal 0.32 and 4.08, respectively. This minimum effect size is higher than previous studies using independent t-test being between 0.00-0.09 8,10,12 because this study uses ANCOVA assisting to control the covariate effect. Thus, the sample size of further study using G power should have at least 40 participants in each group to achieve significant outcomes.
The ASE Program demonstrated greater perceived self-efficacy for exercise, improving blood sugar level (HbA1c), reducing waist circumference, and increasing skeletal muscle. Accordingly, the ASE program ought to practically be integrated as a part of a lifestyle modification program for persons with T2DM in order to increase exercise in daily life and promote successfully well-controlled diabetes leading to prevent diabetes complications and improve quality of life. Furthermore, further studies should be conducted in relation to the ASE Program comparing frequency of exercise and integrating food control over 6-12 months for better health outcomes.
Thanks are extended to the School of Nursing, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Thailand for the grant supporting this study and also participants for their participation.