Thailand is an agricultural country including approximately 19.4 million farmers, ranking at a top twenty in the world.1 This tropical area has outbreaks of insects; consequently, many farmers use insecticide Organophosphate and Carbamate are two types of insecticide that are commonly used by Thai farmers.2 Farmers are directly exposed to insecticide through their breathing, oral cavity, and skin due to inappropriate mix of insecticide at a mixing stage, long term duration and frequency of application, an inappropriate application method, and inappropriate use of personal protective equipment.3 These insecticides have effects on environment’s imbalance, over cost, and health. The insecticides will be absorbed into the bloodstream to inhibit functioning of the cholinesterase enzyme that transmits nerve signals to different major organs in the body. The effects of insecticide on health can be both acute and chronic. Acute effects include nausea, vomiting, headache, muscle pain, diarrhea, difficulty breathing, and blurred vision, while chronic effects are cancer, diabetes mellitus, paralysis, skin disease, infertility, and birth defects in newborn infants. Excessive exposure to insecticide can cause mortality.2,4 Thus, the amount of blood cholinesterase should be measured to detect and diagnose organophosphate insecticide exposure or poisoning, and used to monitor increased risk of exposure to organophosphate compounds.5
Previous studies have revealed that most farmers have knowledge, but they lack awareness and continue to have inappropriate use of insecticide. For example, they may prepare the insecticide using more chemicals than the recommendation on the product labels. Moreover, they may not wear gloves while preparing or applying insecticide, or they may smoke cigarettes when they are spraying insecticide on their farm. The farmers may not immediately wash their hands or take a shower after they are exposed to insecticide or before they eat. In addition, they may blow the spray head using their mouth. Furthermore, they may not put up a sign to warn other people that insecticide has been sprayed in the areas, or they may destroy the insecticide containers with incorrect methods.6-8
Most of previous intervention studies emphasized behavioral modification on an individual level. Contamination of exposure in the community environment persisted, and community members lacked cooperation in the prevention program. Therefore, it has been recommended that community participation should be integrated into the insecticide exposure prevention program.9,10 Some studies have utilized the participatory framework to assess community participation, and participatory action research has shown that farmers have more appropriate use of insecticide which could be further promoted to ensure sustainability of the practice.11,12 Most previous studies tested effects of insecticide exposure prevention programs by reactive paper with low reliability.
Prachuabkhirikhan and Ratchaburi Provinces are located in the western region of Thailand. Most people are farmers, growing radish all year round with continuous use of insecticide; therefore, the screening for blood cholinesterase levels with reactive paper by Sub-district Health Promoting Hospital was positive, indicating that they are at risk of increasing susceptibility to insecticide exposure. As community nurse practitioners who proactively work to promote health in farmers and protect them from harms caused by insecticide, in compliance with the policy of the health clinic, the researchers were interested in integrating the conceptual framework of quality of health care by Donabedian13 into the RAMA Model developed by Noppawan Piaseu.14 The model includes raising community awareness, aiming at target outcome, mobilizing change and innovation, and assuring synergy so as to ensure changes to promote health and prevent exposure to insecticide among farmers, at an individual family and a community level.
Design, population and sample
The study was quasi-experimental research with a two-group pretest-posttest design. The study participants were 49 radish farmers exposed to organophosphate in the west of Thailand. The control group included 24 participants living in Ban Ka Community under the responsibility of Ban Ka Sub-district Health Promoting Hospital, Ratchaburi Province. The experimental group included 25 participants living in Ban Nerntakian Community under the responsibility of Huay sai Ngam Sub-district Health Promoting Hospital, Prachuabkhirikhan Province between April and July 2016. The farmers in these two settings grow radish and use the same type of insecticide.
The samples were recruited through convenience sampling with the following inclusion criteria:
1) they were aged between 20 and 59 years old, 2) with continuous use of organophosphate at least three months, 3) with intensity of insecticide exposure, 4) they had no chronic illnesses, were not pregnant or were not breastfeeding, 5) they did not use medication or herbal medication in the anticholinesterase group, and 6) they had good consciousness and signed a consent form after receiving the research information.
The sample size was determined based on Power Analysis using G*Power statistics with power of test at 0.80, p-value at 0.05, effect size at 0.80 according to a previous study15 obtaining a sample of 21 participants per group. Approximately 20% were added, obtaining the final sample of 25 participants per group. However, there was one participant in the control group who did not have a blood test.
Instruments
The instruments used in this study were divided into three parts as follows:
Part 1: Instruments for screening
The farmers’ insecticide exposure screening questionnaire was modified from the insecticide survey questionnaire by Sirivarasai et al.16 with insecticide exposure intensity algorithm of Agriculture Health Study.3 The questionnaire was divided into three parts: 1) demographic characteristics of the participants, 2) the insecticide use, and 3) the intensity of insecticide exposure including preparation of insecticide, application of insecticide, maintenance of insecticide, and use of protective equipment. The instrument was submitted to a panel of three experts in toxicology, occupational health, and advanced nursing practice. The instrument was then revised and improved based on the experts’ comment and suggestions. The content validity index (CVI) was equal to 0.95. The questionnaire was tried out with 30 farmers. The test-retest reliability with a two-week interval was 0.99.
Part 2: Instruments for data collection
1) The farmers’ insecticide exposure assessment questionnaire was modified from the farmers’ insecticide exposure risk assessment questionnaire developed by the Ministry of Public Health, Department of Disease Control, Bureau of Occupational and Environmental Diseases.17 The questionnaire was divided into three parts: 1) duration and frequency to insecticide exposure, 2) insecticide exposure in work practices consisting of nine negative items and ten positive items, totaling 19 items. The response choices included behaviors with low risk, moderate risk, and high risk. Reverse scoring was used with positive items. Possible total scores ranged from 19 to 57, indicating low risk of exposure to insecticide (19-28), moderate risk of exposure to insecticide (29-38), and high risk of exposure to insecticide (39-57), and 3) the illness or abnormal symptoms that occurred after exposure to insecticide with responses including mild, moderate, and severe symptoms. The CVI was 0.95. The test-retest reliability with a two-week interval was 0.99.
2) Equipment used in laboratory for measurement of blood cholinesterase was Cobas 6000 (C501) with colorimetric assay. 18 Cholinesterase catalyzes the hydrolysis of butyrylthiocholine to thiocholine and butyrate. Thiocholine instantaneously reduces the yellow hexacyanoferrate (III) to the almost colorless hexacyanoferrate (II). This decrease in color can be measured photometrically. For this technique, within-run precision (CV) was determined using human samples and controls in an internal protocol with repeatability (n = 21) and %CV was 0.5. Between run precision (CV) was ranged from 0.9 to 2.6%, with a mean of 1.4 %.
Part 3: Instrument for experiment
The 12-week Insecticide Exposure Prevention Program was adapted from the quality of health care model by Donabedian13 and the RAMA Model.14
Based on Donabedian, 13 the structural components were 1) radish farmers, 2) farmers’ families, 3) Ban Nerntakian Community members, 4) community leaders including Sub-district Administration Organization board members and head of the village, 5) stakeholders including owners of stores selling insecticide and protective equipment and owned agricultural land, 6) resources including farmer group, village fund, and staff members of the Department of Agricultural Promotion in Hua Hin District, 7) a health team including village health volunteers, community nurse practitioners, and public health of Sub-district Health Promoting Hospital, 8) the policy on farmers’ health clinic, and 9) the environment and cultures in Ban Nerntakian Community.
The process of the program was based on the components of the RAMA model: 1) Raising awareness included a group process at the individual and family levels, and a focus group with community leaders, stakeholders, supporters, and healthcare team, 2) Aiming at target outcome included community participation aiming to determine a problem and set a mutual goal to protect insecticide exposure in community, 3) Mobilizing change and innovation consisted of group activity aiming to promote the use of protective equipment, demonstrate role model, encourage positive reinforcement and exchange experiences and process innovation to prevent insecticide exposure, and 4) Assuring synergy involved home visits by health team, prevention of insecticide exposure toward the community rules, and management of the problem.
The outcomes of the program were lower insecticide exposure levels and higher blood cholinesterase levels. The instrument was submitted to a panel of three experts to ensure content validity and appropriateness of the language. The instrument was then revised and improved based on the experts’comments and suggestions. The CVI was 0.95.
Preparation stage
After the research proposal was approved by the Institutional Review Board on Research Involving Human Subjects of the Faculty of Medicine, Ramathibodi Hospital, Mahidol University, the researchers contacted the head of the Tambon Administration Organization, Tambon Health Promoting Hospital, and the District Agricultural Office to explain the study objectives and ask for permission to conduct the study. The researcher then organized a meeting to ask for cooperation and prepare the healthcare team including public health volunteers, community nurse practitioners, and public health officers of Ban Huay Sai Ngam Sub-district Health Promoting Hospital who were research assistants. The researchers surveyed and gathered data regarding demographic characteristics of Ban Nerntakian community as well as established rapport with the community before the study commenced. The media and equipment for program implementation such as pictures, flip charts, experimental luminol, and a farmers’ manual were also prepared.
Data collection stage
After the consent was given, the farmers who met the inclusion criteria were asked to complete the self-reported insecticide exposure assessment questionnaire, lasting approximately 10 minutes, then a blood test was done for a baseline cholinesterase level.
Control group : The researcher distributed the farmers’ manual and made an appointment for a meeting 11 weeks later. During weeks 1 to 10, the participants in the control group were told to live their life as usual, with similar use of and protection from insecticide as they normally did. They also received routine nursing care. In week 11, the control group were asked to respond to the farmers’ insecticide exposure assessment questionnaire and their blood sample was taken for determination of levels of blood cholinesterase in the laboratory. In week 12, a group activity was carried out to raise their awareness and change their exposure to insecticide. The researcher gave the control group a token of appreciation which was a protective gear to prevent insecticide exposure. Then, the data regarding these participants’ exposure to insecticide and their levels of blood cholinesterase were sent to the farmers’ health clinic of Tambon Ban Ka Health Promoting Hospital for their follow-ups to reduce and prevent insecticide exposure (Diagram 1).
Experimental group : The 12-week insecticide exposure prevention program was implemented (Diagram 1):
Raising community awareness aimed at raising the awareness of individuals, their family, and the community, lasing two weeks. In the first week, the activity was at the individual and family level. The data regarding levels of risk and severity of insecticide exposure derived from the blood cholinesterase test in the laboratory as well as the test with a reactive paper were interpreted and given to individual farmers in the experimental group. Then, the group process was utilized to stimulate the participants’ perception of risks, severity, and dangers from unprotected use of insecticide using pictures,flip charts, and experimental luminal to simulate situations that reflect risks of insecticide exposure from their agricultural work. This activity enabled farmers to become aware of the risks they and their family were facing. They discussed the dangers and asked about preventive measures to reduce their risks of insecticide exposure. In week 2, the awareness of the community was raised. A group discussion was held with community leaders, stakeholders, resources, and healthcare team members in attendance. The researcher presented the overall information of the results of risk assessment and statistics on past problems caused by exposure to insecticide by the healthcare team. The participants’ perception of extent and severity of the problems and understanding of dangers of insecticide and unprotected insecticide exposure was stimulated so that the community members would become aware of the danger of exposure to insecticide in the environment, hence cooperation with the campaign to promote insecticide exposure prevention in the community.
Aiming at targeted health was conducted in week 3 by organizing a participatory action to enable community members to collaborative determine problems and obstacles and search for solutions. It was found that the community lacked sources of support and some of the protective equipment was not available in the community, particularly effective filter masks. The community set a mutual goal to use protective equipment every time they used insecticide and to use insecticide with care.
Mobilizing change and innovation was undertaken in week 4 when the researcher coordinated with a source of support who provided a filter mask for farmers to try. Also, a group activity was conducted to demonstrate how to correctly and completely use protective equipment. The participants were given an opportunity to exchange ideas and attitudes toward prevention of insecticide exposure. The farmers who were role models of users of protective equipment to prevent exposure to insecticide joined the idea-sharing activity for positive reinforcement and exchange of experiences, with the aim to stimulate farmers who had never used protective equipment before to have behavioral modification. Furthermore, the innovative policy on prevention of insecticide exposure in the community was promoted. For example, farmers were encouraged to make a covered water container available at all radish patches so that they would be able to rinse themselves immediately after each exposure. Also, a friend mutual support system was devised so that farmers could remind fellow farmers to correctly wear protective equipment every time they sprayed insecticide, and an examination of environmental insecticide was proposed with support of budgets and equipment from the community leaders and available resources in the community. The innovation for environmental safety enabled community members to become aware of harms caused by use of insecticide and to be eager to participate in insecticide exposure prevention activities.
Assuring synergy activity involved implementing the plan of the community and conducting of home visits by the researcher and the healthcare team members to offer consultancy and encouragement to farmers. The farmers’ comments and suggestions were recorded, and the changes were observed and assessed. In weeks 5 and 6, it was found that after behavioral modification regarding insecticide exposure in the first two weeks, 32% of the participants began to completely use protective equipment and 28% prepared a covered water container in their vegetable patches. Such information was used at the participatory action in week 7 to collaboratively analyze and evaluate the outcomes and search for further solutions. As a result, a more clearly-defined practice guideline for the community was derived. In addition, the participants gave one another encouragement and support to use protective equipment to prevent insecticide exposure and protect their own health. In some vegetable patches, there were natural ponds that the farmers used to wash their body. It was recommended that trees should be grown along the edge of the ponds to prevent contamination of insecticide droplets in the ponds. The practices specified in the plan were additionally conducted. In weeks 8 to 10, the researcher and the healthcare team members conducted home visits every other week. The evaluation showed that the farmers had better behaviors when it came to prevention of insecticide exposure. The percentage of those who fully wore protective equipment increased to 44%. However, 56% of them did not fully wear protective equipment, particularly the boots, because the soil was sticky and slippery, but they immediately washed their body after spraying insecticide. All of them had a lower level of exposure to insecticide compared to the level assessed before the experiment started. In week 11, the participants in the experimental group were asked to complete the farmers’ insecticide exposure assessment questionnaire and the blood sample was taken to determine the levels of blood cholinesterase in the laboratory. In week 12, a community participatory meeting was held to give the community members an opportunity to evaluate the operational outcomes and reflect on problems and obstacles they had to overcome to accomplish their goals in weeks 8-10. After that, the researcher presented the outcomes of the insecticide exposure prevention program and the statistics on levels of exposure and blood cholinesterase of farmers. The community members were asked to analyze the outcomes and propose recommendations and agreements to better suit the actual contexts of Ban Nerntakian Community. The researcher gave the experimental group a token of appreciation which was a protective gear to prevent insecticide exposure. Finally, the data regarding these participants’ exposure to insecticide and their levels of blood cholinesterase were sent to the farmers’ health clinic of Tambon Ban Huay Sai Ngam Health Promoting Hospital for their follow-ups to ensure sustainability of insecticide exposure prevention.
Unexpectedly, during the data collection process, the experimental group experienced the insect outbreak, therefore, they used insecticide more frequently.
Statistical analysis
Descriptive statistics of number, percentage, frequency, mean, median, range, and standard deviation were utilized to analyze data regarding demographic characteristics of the participants. Moreover, Chi-square test and Fisher’s Exact test were employed to analyze differences in demographic characteristics of nominal scale variables between the experimental group and the control group, while Mann- Whitney test was used to analyze differences in demographic characteristics of ratio scale variables between the experimental group and the control group. In addition, the Paired t-test was utilized to compare the means of levels of exposure and blood cholinesterase of farmers in the experimental group before and after the insecticide exposure prevention program. Finally, the Independent t-test was used to analyze the differences in demographic characteristics of ratio scale variables with normal distribution between the experimental group and the control group as well as to compare mean differences of levels of exposure and blood cholinesterase between the experimental group and the control group after the insecticide exposure prevention program.
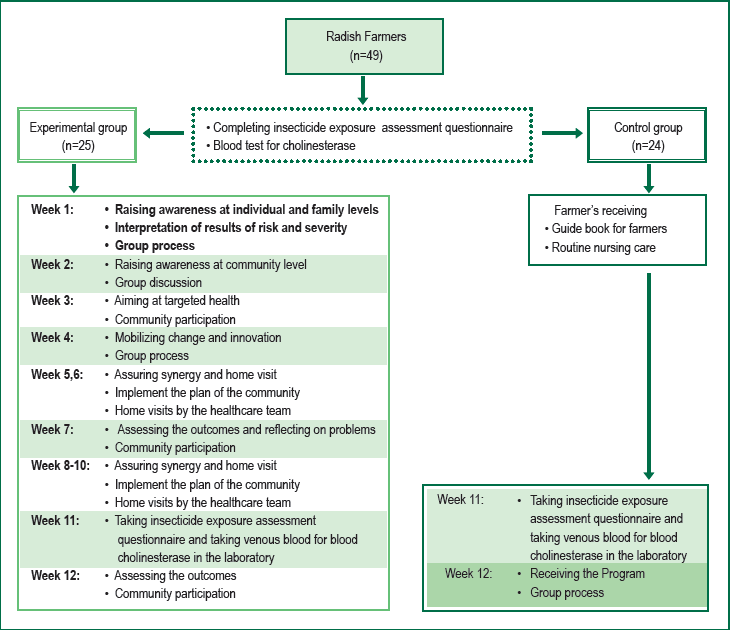
Figure 1: Data collection process
Part 1: Demographic characteristics of the participants
Results revealed that the mean age of the experimental group was 37.04 years (SD = 6.74) and that of the control group was 37.71 years (SD = 9.90). There were more male farmers in the experimental (72%) and the control (70.8%) groups. The insecticides used by the farmers were organophosphate, avermectin, pyrazole, phenylpyrazole, and chloroacetamide. Most of the samples had been using these insecticides for 6-10 years, 3-4 times a week. The participants’ characteristics were not statistically different between the experimental and control groups.
Part 2: Levels of insecticide exposure and blood cholinesterase of farmers in the experimental group before and after the program
The experimental group had insecticide exposure levels at 38.52 before and 28.80 after the program. The paired t-test showed that after the program, the experimental group had less insecticide exposure level when compared to that before the program (t = 10.924, p < 0.001). The experimental group had blood cholinesterase levels at 7.01 before and 6.59 after the program. The paired t-test showed that after the program, blood cholinesterase levels of the experimental group were not significantly different when compared to that before the program (t = 1.315, p = 0.201) (Table 1).
Part 3: Levels of insecticide exposure and blood cholinesterase of farmers in the experimental group and the control group before and after the program
Since the mean scores of insecticide exposure between of the experimental (38.52) and the control (40.83) groups were significantly different before the program (t = -2.135, p = 0.038), mean differences between the experimental and the control groups were compared using independent t-test revealing that mean difference of insecticide exposure was higher in the experimental (9.72) group than the control (2.63) group (t = 6.612, p < 0.001) (Table 2).
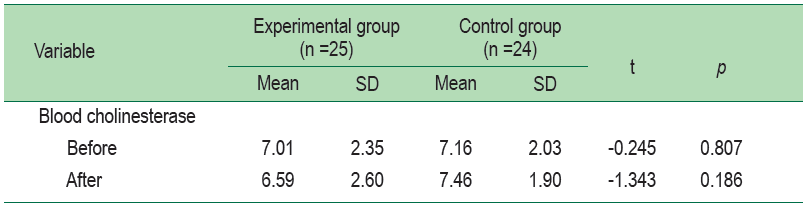
Blood cholinesterase levels of the experimental and the control groups were 6.59 and 7.46, respectively. The independent t-test showed that after the program, blood cholinesterase level in the experimental group was not significantly different from the control group (t = 1.343, p = 0.186) (Table 3).
Table 1: Comparison of insecticide exposure and blood cholinesterase of experimental and control groups. (n = 49)
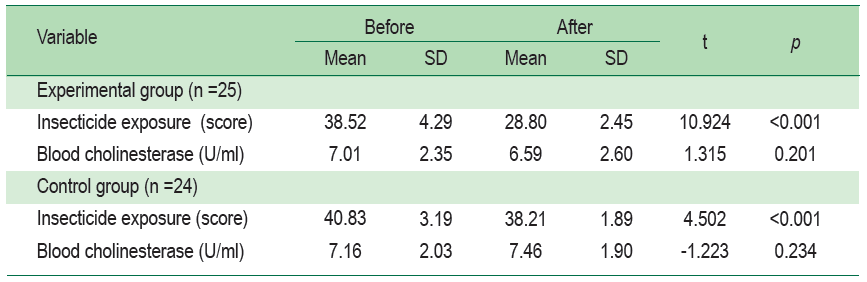
Table 2: Comparison of the mean difference level of insecticide exposure between experimental and control groups. (n = 49)
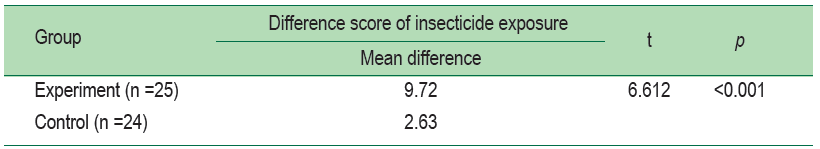
Table 3: Comparison of the mean blood cholinesterase between experimental and control groups. (n = 49)
The results of this study partially support the hypotheses as follows. After the program, the experimental group had lower insecticide exposure levels than before the program and the control group with statistical significance. It is possibly due to behavioral change based on the quality of health care as described by Donabedian13 and the process following the RAMA model as described by Piaseu.14 The community participation and group discussions could raise awareness and stimulate the structural components of the community to cooperate and support the Program. This is consistent with Noosorn et al.19 The activities that raised awareness at individual and family levels through interpretation of risk and the consequence. The group process that enhanced dissemination of knowledge and perception enabled farmers to have better knowledge and practices of insecticide use and exposure prevention. These findings were congruent with Muanmart et al.,20 and Forster-Cox et al.21 The aim at the targeted health outcome could be achieved with distribution of the targeted groups, consideration of the local contexts, long-term campaigns, goal-settings based on previous experiences, and goal-setting at a group level, similar to a previous study conducted by Feola&Binder22 that is sustainable. The mobilization changes activities through group processes, demonstrating and training use of protective equipment equipped farmers with necessary knowledge and attitude and enabled them to have more use of protective equipment. Such findings were consistent with Charoensuk23 and Macfariane et al.24 Furthermore, the innovation community policies were promoted to collaboratively prevent insecticide exposure and check environmental insecticide to further increase the awareness of the community members. The assuring synergy activities through implementing the plan of the community and home visits by the healthcare team. The findings of this study are similar to the results from previous studies.25-27 However, after the program, the blood cholinesterase level in the experimental group was not statistically different from before the program and the control group. This was consistent with the finding of Somboon.15 because of history effects, the experimental group experienced an insect outbreak. The farmer used insecticide more frequently and used more types of chemical which is associated with the level of blood cholinesterase.28,29
While the control group did not experience the insect outbreak, they were slightly reduced. Therefore, the control group may have changes in their blood cholinesterase levels.5
Limitations of the Study
The limitations of the study were as follows:
Strengths of the Study
The present study emphasized collaboration in the community. Awareness of individuals, their family, and the community was raised, and the innovation of the environmental insecticide measuring technique made the community eager to set a mutual goal to prevent insecticide exposure, hence a tendency toward desirable outcomes.
Recommendations
Based on the study findings, the following recommendations could be made:
The results suggest that community nurse practitioners apply the principle of raising awareness, aiming at target outcome, mobilizing change and innovation as approaches for insecticide exposure prevention program in the “farmers’ health clinic”, along with outcome monitoring for sustainability.
This research was supported by the King Prajadhipok and Queen Rambhaibarni Memorial Foundation, the Royal Bangkok Sports Club, the Potential Development of Thai People Project, and the Faculty of Medicine Ramathibodi Hospital, Mahidol University. And I would like to thank Ban Ka and Ban Nerntakian Community health teams in Sub-district Health Promoting Hospital for their help and contributions to this successful research.