Thalassemia and hemoglobinopathy are hereditary diseases that cause chronic hemolytic anemia leading to many physiological adaptations and pathological effects with multiple organ dysfunction.1-4 Heart disease is a major source of mortality and morbidity in patients with thalassemia,5 despite improved prognosis with iron chelation. The common cardiac problems are cardiac hypertrophy, ventricular systolic dysfunction, pericarditis and PH.6,7
Many features of cardiac disease in thalassemic patients are still poorly understood. Cardiac complications are multifactorial and may be due to chronic anemia, iron overload, and probably various other mechanisms.8,9 It has been noted that some patients with severe forms of thalassemia have a burden of right heart strain resulting from PH, iron overload, or small pulmonary emboli.10-16
Thalassemia heart disease affects mainly left ventricular (LV) dysfunctions caused by transfusion-induced iron overload. However, recent studies refer that thalassemia major and thalassemia intermedia patients have an exceptional hemodynamic pattern consistent with right ventricular cardiomyopathy and PH, in addition to the left ventricular abnormalities,17 and can be a leading cause of heart failure in these patients.
Studies in thalassemia show that adults frequently have undetected PH, with a prevalence of 60-70% reported.18,19 Although most of the reported thalassemic patients with PH were splenectomised,6,20,21 non-splenectomised patients were also found to have PH.6 Advanced age and a history of splenectomy are major risk factors for PH in this population.20-25 Since strict compliance with chronic transfusion and chelation therapy to prevent iron overload cuts the condition of heart failure, and prevents PH,26-28 insufficiently transfused thalassemia patients may be at higher risk for the development of PH.
Treatment of thalassemia major consists of constant blood transfusions and iron chelation therapy, which can delay cardiac complications and improve longevity. Early studies showed notable improvement of survival rates and good prognosis from treatment with chelating agents and regular transfusion.29,30 even in severe cardiomyopathy, which may be due to accumulation of iron within myocytes,31 which may be reversed by treatment with iron chelators.32,33
Frequent monitoring of cardiac function in transfusion- dependent patients may identify those at risk of developing future cardiac problems, who might then be candidates for more intensive and sustained iron chelation therapy
The development of the T2* parameter using cardiac magnetic resonance (cMR) scanning has provided a powerful tool for assessing tissue levels of iron and has contributed to the recently observed decrease in deaths from cardiac iron overload.34 Despite the importance of cMR scanning and T2* assessment of tissue iron content, the scan is quite expensive and not available generally. Transthoracic echocardiography (TTE) is widely available at low cost. For many countries the backbone of assessing cardiac involvement in thalassemia has been by TTE. This technique is widely available and has the advantage of being applied at the bedside.
To the best of our knowledge, no studies exist of PH and right ventricular function in splenectomized and nonsplenectomized thalassemic patients who have supposedly received adequate treatment with blood transfusion and iron chelating agents. We speculated that there would be differences in echocardiographic indexes.
Our study aims to determine PH and right ventricular function by using conventional, tissue doppler imaging and a novel echocardiographic technique in thalassemic patients.
Study population
The study population included 32 asymtomatic thalassemic patients (16 male, 16 female; mean age 40.43±14 years). Inclusion criteria: diagnosis of beta thalassemia; normal renal function; asymptomatic; no prior history of admission with heart failure; and an absence of congenital or acquired structural heart or lung disease. All thalassemic patients received regular follow-ups at out- patient hematologic clinic department, faculty of medicine, at Ramathibodhi Hospital, Mahidol University. Cardiac evaluations of all patients were performed after they had visited the hematologic clinic. The laboratory requirements were collected at the same time. Informed consent was obtained and the study was approved by the Institutional Ethics Committee.
Echocardiography
Conventional, tissue doppler imaging and speckled tracking echocardiography (ARTIDA, Toshiba) were performed by an experienced cardiologist. Conventional echocardiographic measurements were done according to the American Society of echocardiography guidelines.36
PH is defined as: a right ventricular systolic pressure (RVSP) of > 40mmHg and/or a mean pulmonary arterial pressure (mPAP) of > 25mmHg.
The two-dimensional strain is a new measurement method. This new measure uses regional and global contractility. However, normative data of the right ventricular function is not available using this method; therefore we collected the value and compared the findings with other methods.
Statistical analysis
The results were analyzed using SPSS for windows 17.0 and descriptive statistics were presented as percentage, means and SDs. Univariate analysis for group comparisons were performed using Student’s t test and Mann-Whitney U tests, where appropriate.
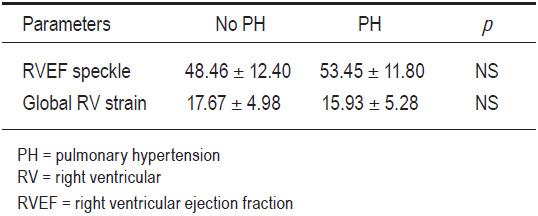
Clinical characteristics and laboratory results of the study group are given in Table 1. All the thalassemic patients had a normal LV systolic function. Echocardiography method; there is no significant differentiation between group and normal value (Table 2). We found a statistically significant difference between the non-pulmonary hypertension group and the PH group in E’, S’ and RV E/E’. In both groups, the myocardial perfusion imaging (MPI) values are abnormal but there is no statistical significance difference between groups (Table 3). A new echocardiography parameter: Global RV strain did not show significant difference between the two groups, though there was a trend of lower global strain in the PH group (Table 4).
Table 1: Clinical characteristics and laboratory parameters of the study group (n = 32).
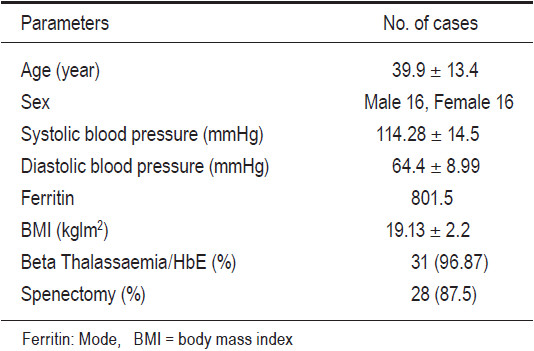
Table 2: Conventional echocardiographic method.
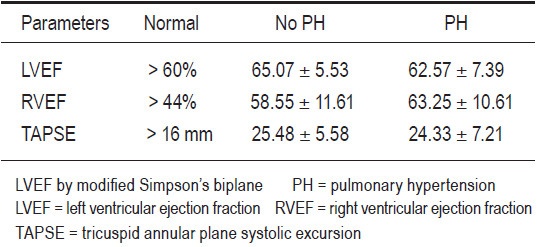
Table 3: Tissue doppler echocardiography of right ventricle.
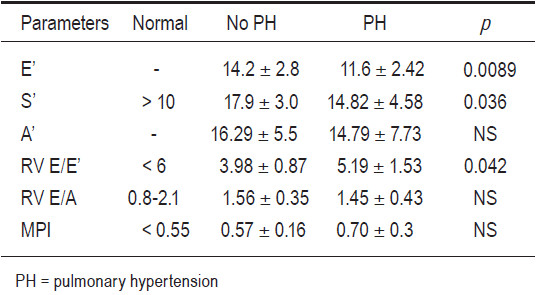
Table 4: Speckle tracking echocardiography of right ventricle.
Cardiopulmonary complications are the main cause of morbidity and mortality in thalassemic patients. In adults with thalassemia pulmonary hypertension is frequently undetected, with a prevalence of 60-70% reported. Thalassemia heart disease affects the left ventricular dysfunction mainly. Thalassemia major and thalassemia intermedia patients have an exceptional hemodynamic pattern consistent with right ventricular cardiomyopathy and PH, in addition to the left ventricular abnormalities that can be a leading cause of cardiopulmonary problems in these patients. Frequent monitoring of cardiac function in patients may indicate those at risk of developing symptomatic cardiac disease, and these patients might then become candidates for more intensive and sustained iron chelation therapy.
The progression of thalassemic cardiomyopathy and PH is a gradual process and the patient is often found to be asymptomatic. Magnetic resonance imaging (MRI) has been shown to quantify myocardial iron content and cardiomyopathy, however, MRI is not widely available and is expensive.
Our study shows that tissue doppler imaging E’, S’ and RV E/E’ parameters are significantly different between those with and without PH in asymptomatic thalassemic patients. A decrease in E’ and E/E’ suggested that RV diastolic dysfunction would be found in those with pulmonary hypertension. S’ velocity was significantly lower in the PH group though it was still in the low normal range. The MPI values in both groups fall in the abnormal range and there was no significant difference. With the speckle tracking technique, we found that the global strain rate was lower in the pulmonary hypertension group though it was not statistically significantly different.
The study’s limitation incudes the small sample volume, it was a cross sectional study, with no comparison to a normal age, sex match control group. If this study is to be extended, we extrapolate that we might be able to see the progress of RV diastolic and systolic function in both groups very clearly.
PH was found in 40% of asymptomatic thalassemic patients. Of all the echocardiographic RV parameters, we found that S’, E’ and TV E/E’ by TDI was the best screening tool to detect early RV dysfunction in asymptomatic thalassemias with PH.