The majority of lung cancer patients present with symptoms at a late stage of the disease, and diagnosis occurs mostly in locally advanced or metastatic disease with poor rates of survival, of up to 5 years. Obviously, the earlier detecting of lung cancer, the better the patient’s prognosis.
The new autofluorescence bronchoscopy can visualize the early change of endobronchial cancer. Autofluorescence bronchoscopy is a procedure in which a blue light rather than white light is employed for illumination and premalignant and malignant tissue is distinguished by a change in color from normal tissue without the need for fluorescence-enhancing drugs.
In 2006, Lam et al1 demonstrated that autofluorescence bronchoscopy could increase the diagnostic yield by 8 percent, (compared with white light bronchoscopy) in patients with abnormal sputum cytology, without patients being subject to additional risk. So far only about 5 per cent of cancer treatment centers in the USA offer this diagnostic tool to their patients.2
This study was to evaluate the benefit of using autofluorescence bronchoscopy for the detection and localization of endobronchial carcinoma.
Between January 2007 and December 2011, autofluorescence bronchoscopy was used to examine 350 patients, aged 35 to 90 years, who were either current or ex-smokers of more than 20 cigarettes per day for up to 20 years. These patients were already suspected to have lung cancer, based on abnormal chest roentgenograms or computer tomograms of the chest, showing for example, minute lung nodules, recurrent pneumonic lesions or elevation of the carcino embryonic antigen (CEA)which is a lung tumor marker.
An autofluorescence bronchoscopy system (model BF-240 bronchoscope; Olympus; Tokyo, Japan) was used. The system was composed of a camera unit, fiberoptic bronchoscopy, excitation light source, and filing system. The white light from the xenon lamp is passed through a cut filter and then through an excitation light. Images obtained with an objective lens were transmitted via a fiber-optic image guide back to the eye piece of endoscope which specifically passed a 490-590 nm fluorescence signal.3 Abnormal mucosa showed a cold image lack of autofluorescence. (Figure 1)
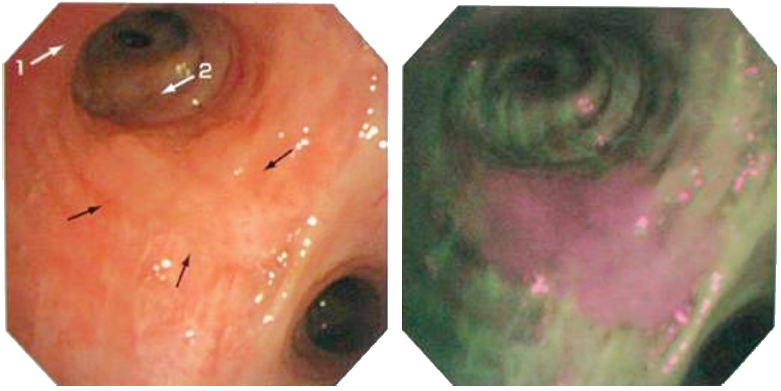
Figure 1: Demonstrates autofluorescence bronchoscopy compared with white light bronchoscopy.
There were 262 men and 88 women with a mean age of 64 years. Premalignant, endobronchial cancer was found in 3 patients; 2 patients in 2008 and 1 patient in 2011. Both patients in 2008 developed carcinoma in situ, which was destroyed by electrocautery. Annual follow ups over the next four years, by autofluorescence bronchoscopy were normal for both. The other patient in 2011 developed severe dysplasia which was ablated by electrocautery. Open lung biopsy of the left lower lobe lesion revealed broncholitis obliteran. In 2008, the patients with lung cancer in our hospital numbered 33 cases, so the aforementioned patients accounted for 6 percent. In 2011, the number of lung cancer patients we treated totaled 53, the previous two existing cases and one new case accounted for 6 percent.
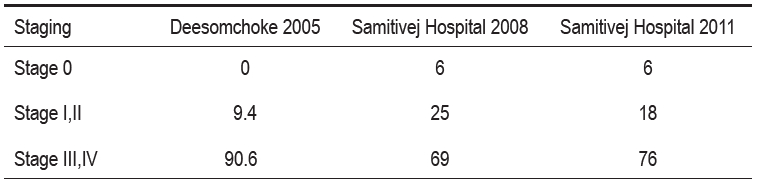
Comparison between the statistics of another hospital in Thailand in 2005, and our own in 2008, demonstrated that we were able to identify early stage of lung cancer cases (Stage 0, TNM classification 2010)4 at a satisfactory rate of 6 percent compared with 0 percent for the other hospital5 ( Table 1).
Table 1: Comparison of staging of the lung cancer in Thailand in percentage.
Additionally, we found that in cases of ablation of invasive endobronchial carcinoma, autofluorescence bronchoscopy enabled us to obtain a more accurate assessment of the lesion size and margin.
Surgery is currently regarded as the accepted treatment of choice of carcinoma in situ and results in 80-90 percent 5 years survival rate.6 For our patients in 2008, one was too old and his lung function test was very poor. The other one developed severe pneumonia. Both received local bronchoscopic treatment with electrocautery, a straightforward and relatively simple procedure, which did not hamper subsequent surgical resection in case of treatment failure. Both patients received annual bronchoscopic examination for 4 consecutive years of follow up and they were cancer free.
There are limitations to the present study. Our results of 2008 and 2011 were compared with the data reported in 2005 from another hospital in Thailand which had no access to autofluorescence bronchoscopy at that time.
The second limitation is that our study populations are small and come from the high income segment of the Thai population, so they may not be representative of the general Thai population who use government hospitals.
Autofluorescence bronchoscopy is able to enhance early detection of endobronchial cancer.