In cases of calf pain and swelling, diagnosis by physical examination alone may be difficult. Emergency physicians will need the history and duration of occurrence as well as routine laboratory findings to help them make the decisiom. Initial investigation may begin with ultrasound, followed by magnetic resonance imaging (MRI). We present a case report of using these systems step by step until the diagnosis was established.
A 67-year-old man, presented to the emergency room (ER) with left knee, calf and ankle pain which developed 2 days prior to admission. His left foot was twisted after a car accident. He subsequently developed severe pain at left knee and leg.
Physical examination
Temperature check revealed low grade fever (T 37.8°C), no dyspnea and normal breath sounds. Left knee was not swollen; ballottement test was negative, limited flexion and extension due to pain. The negative Lachman test indicated neither rips, tears nor palpable mass was detected. Left calf was mildly swollen, and tender. No pain or resistance in the calf was observed during passive ankle dorsiflexion. Left ankle was mildly swollen and tender but it was full range of motion (Figure 1a-b).

 Investigations
Investigations
Routine laboratory test was unremarkable. The clinical differential diagnosis was cellulitis of left calf and deep vein thrombosis (DVT). Hemocultures were taken and intravenous antibiotics (Rocephin® and Clindamycin®) were administered immediately
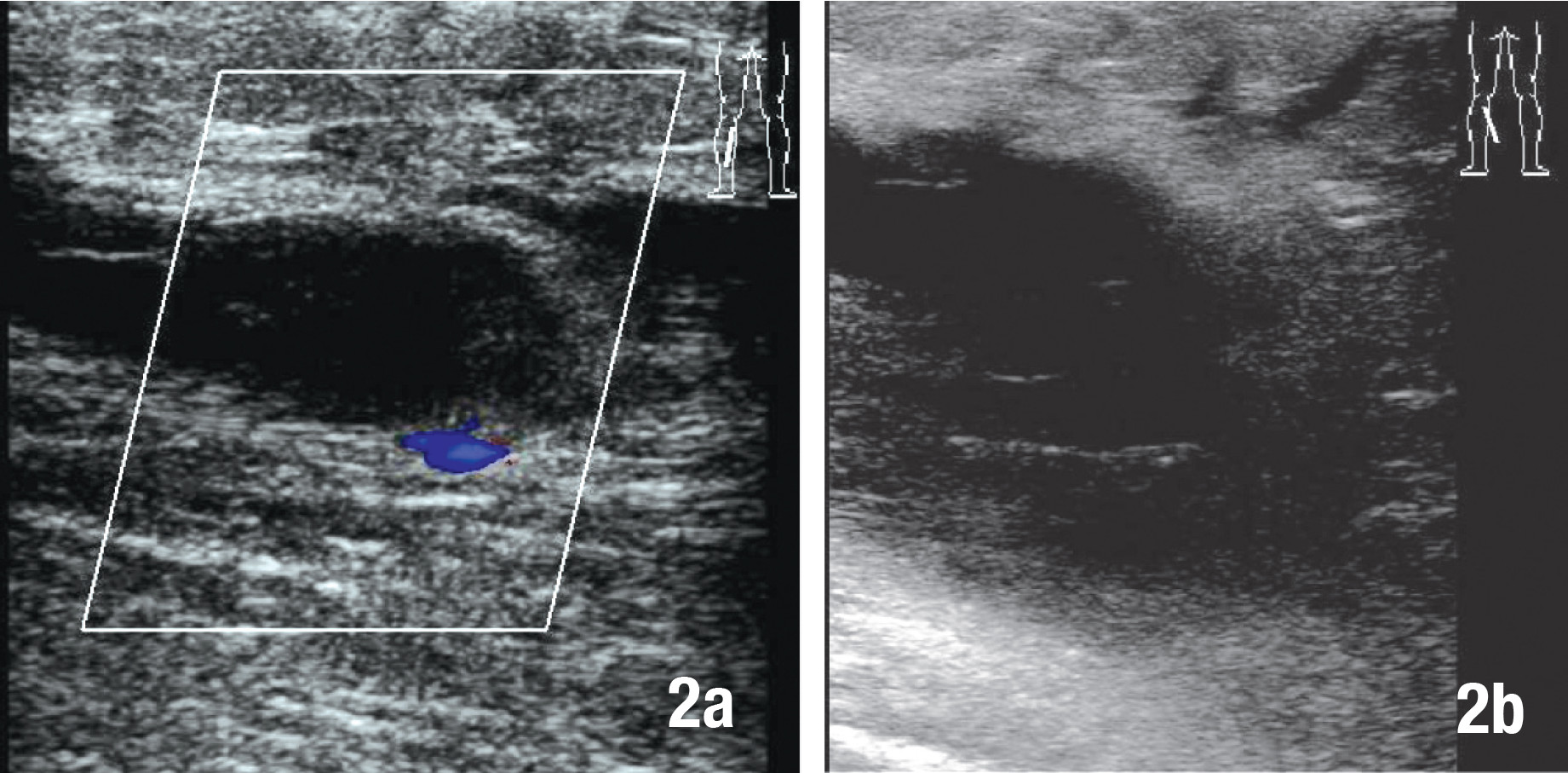
Ultrasound of left leg revealed a echogenic mass at popliteal fossa (Figure 2a). The popliteal vein was compressed by a cystic mass (Figure 2b).
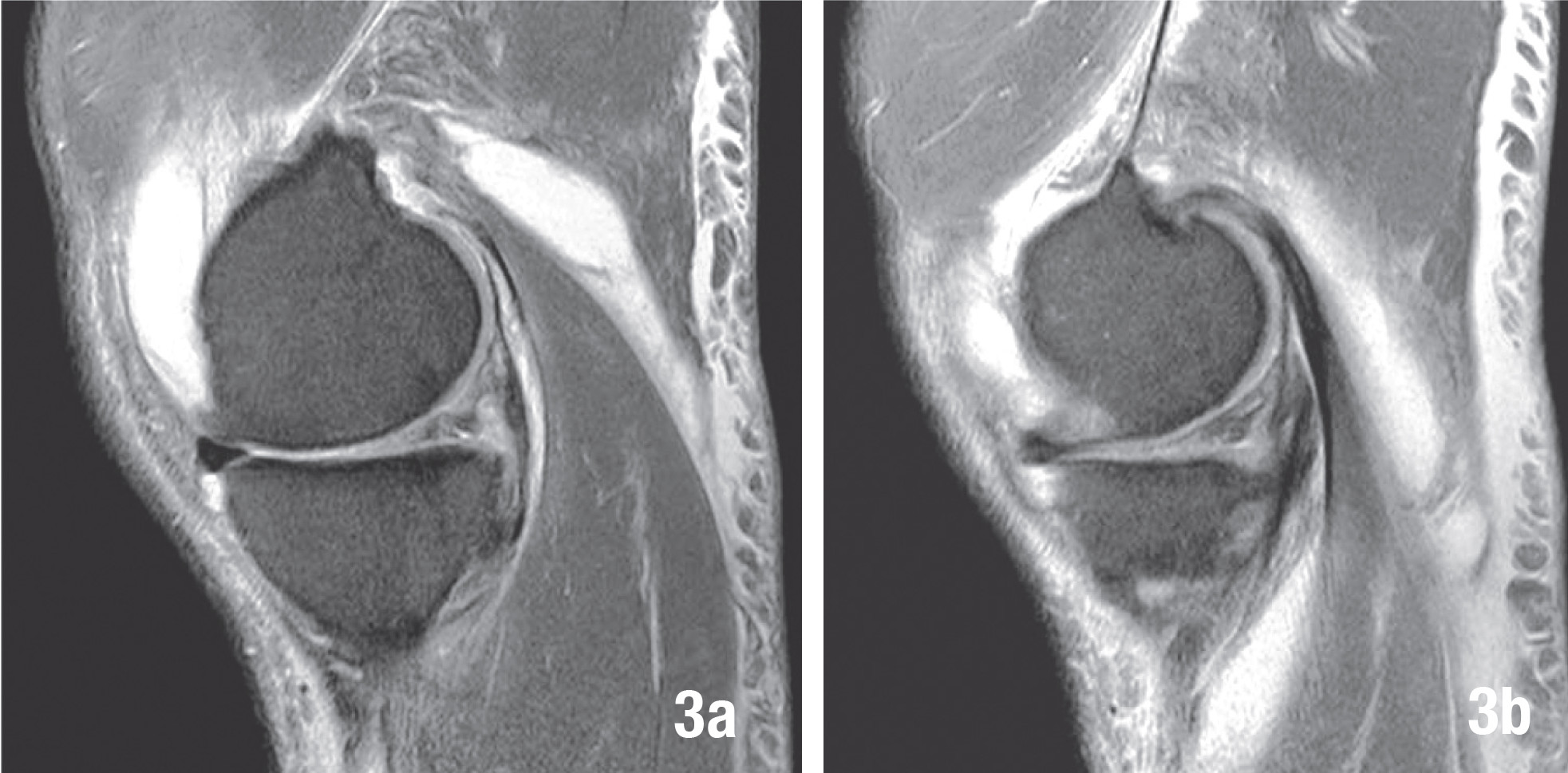
Axial proton density weighted MRI with fat saturation (Figure 3a-b) revealed high signal intensity fluid in the popliteal cyst (Baker’s cyst) which was located between medial head of the gastrocnemius muscle and the semimembranosus tendon. There was extension of high signalintensity fluid inferiorly from the popliteal cyst which surrounded the medial aspect of medial head of gastrocnemius muscle. These fluids dissected subcutaneous tissue of medial aspect of calf and fascia of medial head of gastrocnemius muscle.
Coronal proton density weighted MRI with fat saturation of left knee (Figure 4a) revealed high signal-intensity fluid dissecting subcutaneous tissue of medical aspect of left calf and downward along fascia of medical head of gastrocnemius muscle toward ankle. The signal intensity of gastrocnemius muscle is intact; no atrophic change is noted. Sagittal protein density-weighted MR image with fat saturation of left knee (Figure 4b) shows high signal-intensity fluid extending inferiorly from the popliteal cyst. Continuation of fluid is seen within subcutaneous tissue of posterior aspect of left knee joint. Dissecting fluid is also extending down toward the ankle joint, moderate tear of posterior horn of medical meniscus is also demonstrated on this study.
Hospital course
Symptomatic treatment was started which included physical modalities such as local heat, analgesics, compression, bandages, and close observation. Hemocultures were positive for gram-positive cocci, so IV antibiotics were continued for 1 week. The fever subsided after 1st day of admission; the knee and calf pain swelling were improved. The patient could ambulate on the 3rd day of admission.
Causes of calf swelling and related pain include muscular strain, cellulitis, fasciitis, thrombophlebitis, Baker’s cyst rupture or rupture of plantaris tendon, compartment syndrome, varicosis, popliteal aneurysm rupture or even neural tumor or malignant histiocytoma. The emergency physician is usually the first person to observe the patient presenting with calf pain and swelling. The physician should examine the leg completely as follows: where is the point of tenderness? Is swelling is localized or generalized? What about skin color; is there any fever? Is there any history of trauma? Do a Diagnostic Tap: is there any serous fluid or blood? The physical examination and lab findings may not be conclusive. In such cases then, ultrasonic scan and MRI can be essential to the definite diagnosis as above mentioned in our case.
The history and duration occurrence may be taken into consideration as well. However though the history of trauma may confirm the diagnosis, minor trauma may not be recognized.
The physical examination in general cannot differentiate a ruptured Baker’s cyst from DVT.1 In rare cases, a Baker’s cyst rupture may develop a crescent shaped hemorrhagic sign at the malleolar region. The ultrasonic scan is the initial investigation to evaluate these symptoms. If the diagnostic tap shows hemorrhage, it may indicate ruptured Baker’s cyst rather than DVT. The next investigations to differentiate between these entities are duplex and conventional ultrasound. Ward EE et al2 commented that sonographic detection of Baker’s cyst is 100% accurate when fluid is identified between the semimembranous and medical gastrocnemius tendons, in communication a posterior knee cyst. Not all causes though could be demonstrated well by ultrasound, so further study would be MRI which will demonstrate ruptured Baker’s cyst and the extent of the disease. The gold standard to demonstrate ruptured Baker’s cyst is arthrography. In any case, ruptured Baker’s cyst as opposed DVT should be diagnosed definitely before the start of treatment since the treatment is completely different for each.
The diagnosis of calf pain and swelling is difficult to diagnose by history and physical examination alone. Many differential diagnoses are possible. To distinguish between ruptured Baker’s cyst vs. DVT requires both conventional and duplex ultrasonic scan and finally MRI for a definite diagnosis as shown by our case.