Fiberoptic bronchoscopy (FOB) is a procedure that pulmo- nologists perform to investigate the airway passages for diagnostic or therapeutic purposes. Patients undergoing FOB are either under local anesthesia or moderate sedation. The type of sedation will depend either on the complexity of the procedure or the time needed by the physician to complete the assessment and or treatment. During moderate sedation, several patients were observed in Bangkok Hospital manifesting snoring and hypopneas or apneas. This prompted our team to carry out further investiga- tions in the diagnosis of sleep apnea.
Obstructive sleep apnea (OSA) is described as the repeated instability of the upper airway during sleep which results in hypopnea or apnea. It is a serious condition that can affect an individual’s activities which in turn can also cause long term health problems. Polysomnography or sleep study has been the gold standard in diagnosing sleep apnea. It typically records the brain wave changes, eye movements, muscle motion, breathing and heart rate and rhythm.1 Once diagnosed, the management of OSA depends on the severity of the condition. Some patients may resort to a mandibular advancement splint, continuous positive airway pressure (CPAP), or surgery. Although sleep studies have been effective, the cost and lack of available sleep laboratories and trained technicians has been a major concern in screening patients suspected of sleep apnea. To compensate, methods such as sleep endoscopy and portable polysomnographic devices supported by sleep questionnaires are used in the diagnosis of sleep apnea.
Over a period of twelve months, from January 2014 to December 2014, a total of ten patients suspected of having OSA and who needed to undergo FOB for other reasons aside from sleep apnea were diagnosed with OSA using FOB and CPAP at the Bangkok Hospital.
Pre-procedure assessment
Each patient received a thorough physical examination with particular attention given to the status of the upper airway. This examination was followed by radiographic imaging (either a chest x-ray or computed tomography scan). When the patient was already required to undergo bronchoscopy for further investigation and or treatment, he or she was then further evaluated for a possible diagnosis of obstructive sleep apnea. The Berlin Questionnaire and the Epworth Sleepiness Scale were used to measure the patient’s risk of sleep apnea. If both the physical assessment and the questionnaire score pointed to a high likelihood of sleep apnea, the patient was informed, and consent was obtained to perform FOB and positive end-expiratory pressure (PEEP) titration of mask CPAP.
FOB and PEEP titration of mask CPAP
The FOB allowed direct visualization of the oropah- rayngeal airways with the patient under moderate seda- tion. This view provided the physician with a clear and direct picture of whether the upper airway was collapsed or if any obstruction were present thus confirming sleep apnea. The FOB was then inserted via the mask CPAP to help titrate and adjust PEEP providing the accurate measurement needed when using CPAP. Post-FOB with mask CPAP, the pulmonologist was then able to perform FOB, diagnose OSA and provide CPAP management with specific PEEP levels.
Post-FOB and PEEP titration of mask CPAP
When a patient displayed upper airway collapse or obstruction during FOB and PEEP titration of the CPAP, an ambulatory sleep study was performed to confirm the diagnosis of obstructive sleep apnea. A full portable poly- somnography was completed and mask CPAP with specif- ic PEEP for treatment was prescribed as treatment. Three months after using CPAP, subjects were asked to come back for evaluation.

Figure 1: The patient with CPAP mask is diagnosed with obstructive sleep apnea.

Figure 2: A direct visualization of closed airway of a moderately sedated patient seen via FOB.

Figure 3: The airway dilates when CPAP was applied to the patient.
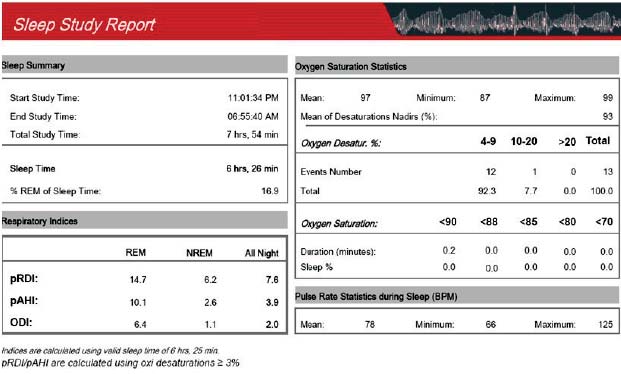
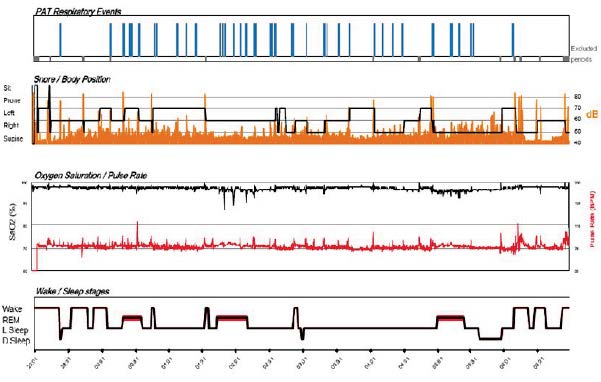
Fiberoptic bronchoscopy and PEEP titration of mask continuous positive airway pressure (CPAP) was performed on ten consenting patients, six of whom were male and four female. The patients’ ages ranged from 35 to 72 years old with a mean age of 51. The mean body weight was 72.8 kilograms (kgs) ranging from 52 kgs to 89.5 kgs. The body mass index (BMI) ranged from 27 to 35 and the mean neck circumference was 18.2 inches. The average PEEP was found to be 7 cmH20 (ranging from 5 to 12 cmH20). No untoward complications were noted from the procedure and moderate sedation. From the sleep study, the mean apnea-hypopnea index (AHI) was 21 events per hour. All the patients had been using CPAP, and tolerated how the machine operates. Nobody reported any difficulty during the follow-up checkup.
Obstructive sleep apnea (OSA) is a serious disorder characterized by repeated collapse of the upper airway when asleep, resulting in reduced airflow or brief absolute airflow cessation when asleep.2 It can present as nocturnal symptoms such as snoring, gasping and apneas observed by bed partners. This condition can also manifest morning symptoms like excessive daytime sleepiness, fatigue, morning headaches, personality changes and other more serious problems such as hypertension,cardiovascular disease,type 2 diabetes mellitus and vehicular accidents.3-8
Diagnostic evaluations play a major role in provid- ing the best treatment options for sleep apnea. A thorough physical examination is very important in diagnosing OSA particularly the BMI, neck and waist circumferences. These clinical features should be integrated with information obtained from sleep questionnaires such as the Epworth Sleepiness Scale and or the Berlin Questionnaire and especially the polysomnography report to accurately diagnose sleep apnea.9
Polysomnography (PSG) or sleep study is a standard diagnostic test that requires the patient to stay in a sleep laboratory to be monitored by a sleep technician8 and may or may not try using CPAP to determine treatment. This method has been considered the gold standard for diagnosing OSA but due to an increase in demand coupled by a lack of facilities and human resources, several techniques have been developed to meet the demands of patients who want to get tested for OSA.
Flemons W et al.10 published a study on the duration of waiting times for the diagnosis of sleep apnea and treatment with CPAP in five countries. Patients from the United Kingdom wait on average from 7 to 60 months for diagnosis and treatment, whereas in Belgium, the wait is 2 months, and in Australia between 3 and 16 months. In the United States waiting time is between 2 and 10 months and in Canada 4 to 36 months. The waiting time varies widely depending on several factors such as the patient’s condition and demographics. This shows that even in more developed countries, there is still a lack of facilities available for patients suspected of having sleep problems. In Asia it is expected that waiting times are even longer, given that the population density is higher, healthcare resources are limited and sleep disorders are not given priority. Furthermore, if a sleep laboratory is used for every presumed case of sleep apnea, waiting times will be longer still.
The study of sleep and the use of CPAP for treatment have evolved in past decades. Recently, sleep study monitoring has been categorized into 4 types.Type I monitors are facility-based with 7 channels; they are run by a sleep laboratory technician, and evaluated by a sleep specialist. Type II monitors are portable, with 7 channels to allow for the identification of different sleep stages and AHI. Type III monitors have 3 to 7 channels but do not assess sleeping and waking stages. Type IV monitors have 1 to 2 channels and do not detect sleep stages nor do they identify the type of apnea, but oxygen saturation is measured.11 To our knowledge, there has not been a complete and comprehensive study to measure the efficacies of each type of sleep study. However, in research published by Dr. Stephanie Su12 comparing PSG and portable home sleep study, it was concluded that there was a significant correlation of respiratory disturbance index (RDI) between the PSG in the labora- tory and ambulatory sleep study. Although mobile sleep tests have their limitations, accompanying reports and physical examination with medical history could prove to be a good alternative for PSG in diagnosing OSA.
Sleep nasendoscopy was introduced by Croft and Pringle in 1991, and requires the patient to be sedated so direct visualization of the airways can be performed while the patient is asleep. This method allows the physician to assess the levels of snoring and or obstruction. Maneuvers and mandibular splints are also applied for further assessment. In a study conducted by Dr. Hohenhorst,13 he stated that drug-induced sleep endoscopy has no known record of severe side effects or life threatening compli- cations. It is a reliable and safe procedure to help diagnose OSA and determine the individual therapeutic choice which could be either surgery or mandibular repositioning appliances. However, polysomnography is still necessary for a complete diagnosis of OSA. In another published study by Dr. Salama,1 it was concluded that sleep endos- copy is a practical procedure in diagnosing OSA. It can also aid in a pre-operative evaluation of patients suspected of OSA.
Sleep nasendoscopy has some points in common with our procedure. Both studies use pharmacological agents in inducing patients to sleep; both visualize the airway using a scope to further investigate the anatomical structure and level of obstruction of patients suspected of OSA. Both procedures do not have records of emergency side effects (considering our study was conducted on patients with comorbidities) and both procedures still require a physical examination, medical history and sleep study results. Several research findings proving the effectiveness and practicality of this procedure have been published. The main difference however, is that after assessment of the airways, CPAP PEEP titration is used to determine if the equipment will function and be useful in dilating the obstruction or narrowed airway of the subjects or if surgery is still deemed necessary. The limitation of this course of action is that it has only been tested on 10 patients, all of whom have responded well to CPAP treatment. Further studies that are more wide scale should now be made to show if FOB with CPAP PEEP titration alone can adequately diagnose OSA without recourse to other studies.
The evolution and widespread availability of inter-ventional bronchoscopy has played a great role in the development of diagnosing certain conditions such as OSA. This new technique is not only practical, cost- efficient, time-saving and beneficial for both patient and physician but it may also be considered as the new gold standard in diagnosing OSA.