Contrast enhanced spectral mammography (CESM) is a technique to detect breast lesions, by determining the pattern of tissue contrast enhancement as well as detecting the extension of the disease. The images are derived from subtraction of dual exposures of low and high x-rays energies after intravenous infection of non-ionic iodinated contrast medium in order to show the enhancement of the lesions. The result is similar to a contrast-enhanced MR of the breast.1 It improves diagnostic accuracy, giving anatomical, pathological and physiological imaging when compared with digital mammography and breast ultrasound.
Technique
-Equipment
The digital mammographic unit is designed for low energy simultaneous dual exposures for a routine digital mammogram and within a second, a high energy exposure for imaging the contrast enhancement of the breast lesion. The two images are automatically and digitally subtracted, leaving only the different patterns of enhanced pathological tissue on the image.
-Procedure
After an evaluation of the patient’s renal function, a rapid intravenous injection is administered at the antecubital vein of non-ionic iodinated contrast medium (300-370mg/ml) in the amount of 1.5ml/kg of body weight, but not exceeding 100 ml. Two minutes or more after the initial injection, the image is taken with the routine positioning for mammography. The simultaneous dual exposures of low and high energy are performed mostly in CC and MLO (or ML) views. The total imaging study time is about 4-6 minutes. Additional views or wash-out patterns may be added. The total x-ray dose per view delivered to the patient averages between 1.30-3.13 mGy1 depending on the breast tissue composition and the thickness of the whole breast.
A 45-year-old female with a history of breast cancer in her sister, with no presenting symptoms, came in for a routine mammography screening.
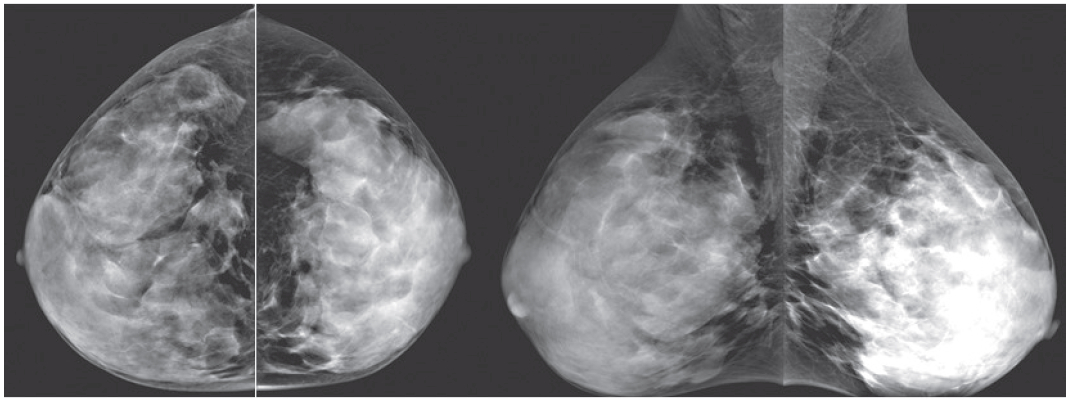
Figure 1A: Digital mammograms in CC and MLO views reveal extremely dense fibroglandular tissue, no detectable convincing lesion.
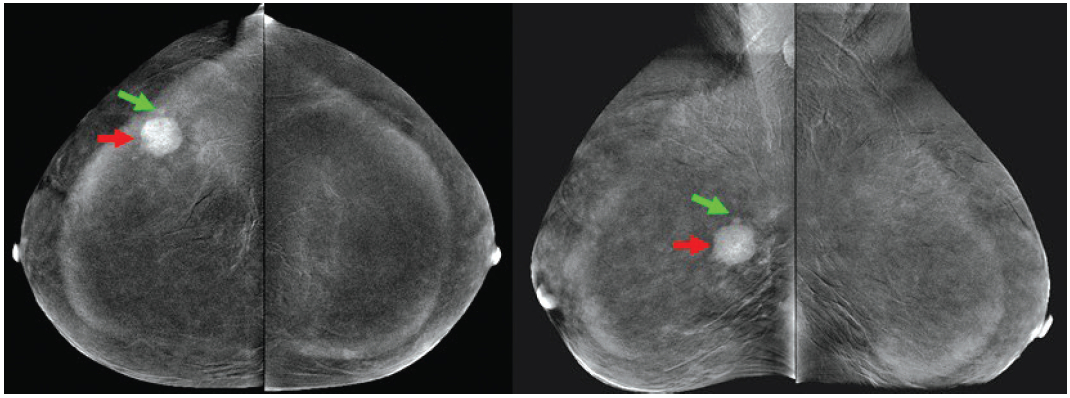
Figure 1B: CESM reveals extensive, inhomogeneous enhancement of a larger microlobulated round mass (red arrow) in outer part of right breast and another nearby tiny foci of enhancement (green arrow). Multiple tiny foci in right breast are not excluded.
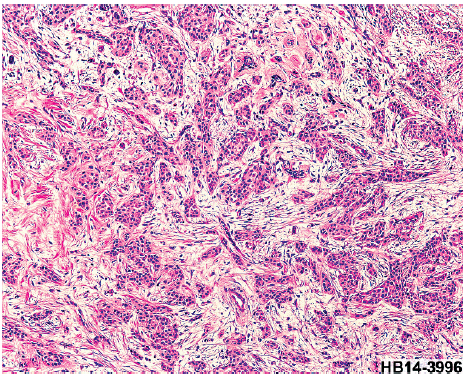
Figure 1C: Core needle biopsy (CNB) reveals invasive ductal carcinoma.
A 60-year-old female had a left total mastectomy; axillary node clearance and TRAM flap operation about two years ago. She presented with pain and palpable abnormality in her post-operative breast.
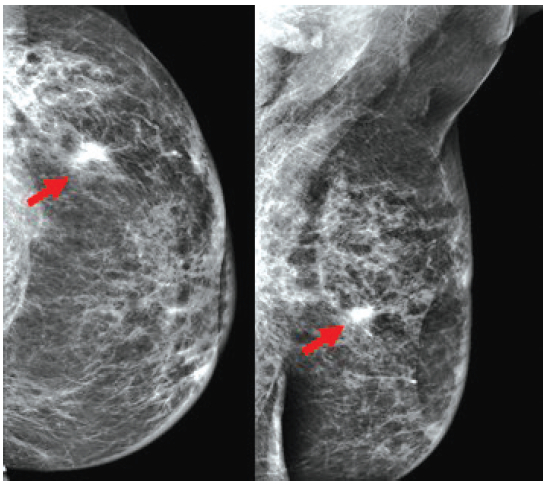
Figure 2A: Digital mammogram in left CC and MLO reveals an irregular shaped hyperdensity mass with spiculation, highly suspected of local recurrence (arrow).
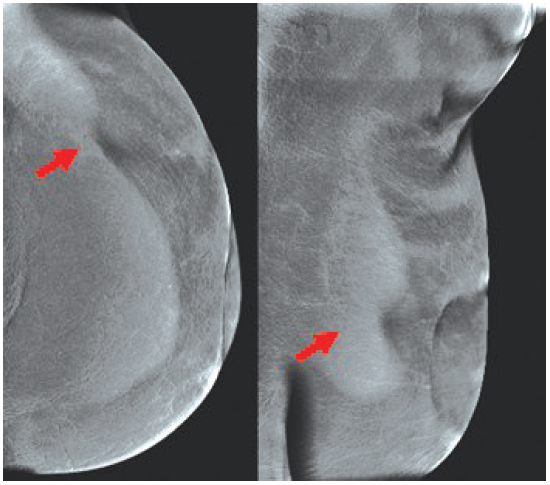
Figure 2B: CESM reveals no abnormal enhancement, particularly in the suspected area (arrow).
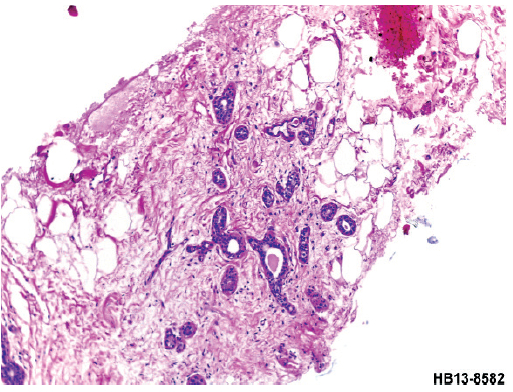
Figure 2C: CNB reveals only a stromal fibrosis. No malignancy is observed.
Within the same breast compression, the low energy exposure gives a low dose; high resolution mammogram followed a second later by high energy exposure. This provides a contrast medium enhancement of abnormal breast lesions. These two images are taken immediately after exposure; meanwhile the automatic direct digital subtraction of the two images is presented immediately on the monitor. The enhancement pattern of the contrast enhanced spectral mammography (CESM) follows the rules of contrast enhanced MRI (CE-MRI). Comparing with CE-MRI, the CESM is expected to show better resolution of a mammography over the MRI resolution (including the presence of microcalcifications and its details, with no motion because both images are obtained in one breast compression of a couple of seconds. The equipment needed for this examination is much cheaper, using the well-known and cheaper iodinated contrast medium. The procedure is fast, not complicated, and similar to routine mammography that includes two views to study both breasts. The procedure takes less time, around four minutes for a capable technician. The CESM examination is not a claustrophobic experience; there are no limitations for overweight patients, or patients with a cardiac pace-maker, a vascular stent, a metallic prosthesis, or old magnetic devices and clips.
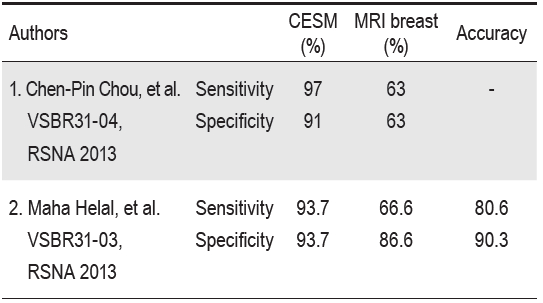
We present a clear case of a malignancy not shown by mammography, but positively identified with CESM (Figure 1). We also present a highly suspected malignancy by mammography which proves negative in CESM (Figure 2). Breast mass is not commonly demonstrable in mammographic examinations of extremely dense breasts. Tomosynthesis cannot add enough information or comparable information for decision of treatment, unlike the CESM results. The extent of the disease is shown in our first case, as there are at least two cancers in one breast, and this result prevented the possibility of conservative breast surgery initially planned for this small mass. The local extension around the cancer can be seen with no difficulty. If there is no enhancement like in the second case, although digital mammography is highly suspicious, the presence of malignancy can mostly be excluded. The enhancement patterns resemble CE-MRI, believed to be the same principle of tumour vascularization and perfusion abnormality of abnormal cells. However, as in CE-MRI, there are the same overlapping patterns of benign and malignant enhancements. Fallenberg EM, et al.2 shows CESM has a better detection rate and size estimation rate than digital mammography. The studies from Chen-Pin Chou, et al.3 and Maha Helal, et al.4 show CESM has a higher sensitivity and specificity than breast MRI (Table 1).
Table 1: Comparison of the sensitivity, specificity and accuracy of CESM with breast CE-MRI.
MRI is beneficial in the differentiation of local recurrence of post treatment scarring after breast conserving therapy, evaluation of residual tumor post treatment, with unknown primary site of malignancy. Recently, the FDA approved the use of MRI in dense breast examinations, which should be replaced by CESM.
Dromain C, et al.5 concluded that CESM improved diagnostic accuracy compared with the use of digital mammography and breast ultrasound. We agree with Dromain, et al. and one of our indications of CESM is to detect which one/ones of the numerous lesions in the breast require tissue study &/or surgery.
However the radiation dose for CESM is higher than digital mammography, ranging from 0.7-3.6 mGy1, per view, almost the same or slightly lower than breast tomosynthesis. There also are untoward side effects of iodinated contrast medium, though this is uncommon in healthy women. Thus we suggest CESM should be performed when there is indication, not as a routine study.
CESM provides higher diagnostic accuracy, providing anatomical, pathological and physiological imaging superior to digital mammography and breast ultrasound. It shares the same principles with CE-MRI, in the enhancement pattern due to the similar uptake of contrast medium or enhancement. Therefore, the indication should be the same. However, CESM had been proved to be more sensitive and more specific than MRI. The image resolution is better than MRI. Microcalcifications are easily detected. There are no limitations as with MRI in regards to the ferromagnetic effect and machine design. It is much more cost-effective than CE-MRI due to the lower cost of equipment, contrast medium and less study time than using routine mammography views. The average time taken in the mammography room is around 4-6 minutes in a routine study. Thus, the patient flow is far better. Furthermore, tele-imaging is also possible.
CESM should be the imaging modality of choice in the detection and extension of breast cancer, particularly in problem cases, or when conservative breast therapy is attempted.