Idiopathic granulomatous mastitis is a relatively rare chronic inflammatory breast disease often mistaken for more common breast disorders, breast abscess or infectious mastitis, and can mimic inflammatory breast cancer.1,2 Since it was first described in 1972 by Kessler and Wolloch3, there have been only 541 cases reported worldwide as shown in a 2011 review article.4 Most patients are women of reproductive age, most commonly aged 22 - 42.5 It frequently occurs two to six years after pregnancy.6 The lesion typically presents as a unilateral firm breast mass and can occur in any quadrants of the breast except in the subareolar area, sometimes with inflammation of overlying skin, abscesses and fistulae.7-10 It usually poses a complex diagnostic and therapeutic dilemma because of the unknown etiology. A tissue biopsy is necessary to confirm the definite diagnosis. It is characterized by noncaseous granulomas and microabscesses confined to breast lobules with the absence of any infection during histopathological evaluation.11,12
Definitive treatment of idiopathic granulomatous mastitis remains controversial.13 The available options of treatment include expectant management, antibiotics, steroids, other immunosuppressive drugs and surgical excision with varying degrees of response and recurrence.2,8,14,15 Long-term follow-up is generally suggested in any treatments due to high rate of recurrence.16,17
In this report we present a patient with bilateral inflammatory breast mass finally diagnosed as idiopathic granulomatous mastitis. We review and discuss the history, clinical presentation, imaging, diagnosis and course of treatments for this disease in this patient who eventually was treated successfully with steroid therapy.
A 44-year-old premenopausal Thai female, gravida 1 para 1, presented with a painful palpable right breast mass for four days, with associated inflammation of the overlying skin. She delivered her only son when she was 38 years old and had breastfed for 3 years. Her menarche was at the age of 13 and from then her menstrual cycles had come regularly. She had no history of drug or food allergy. Also, no history of smoking and previous use of oral contraceptives or any hormone was detected. Her past medical and surgical histories were unremarkable, without any breast disease, surgery or recent breast trauma. Her family history was negative for both breast cancer and autoimmune disease along with no recent tuberculosis exposure. Systemic review was normal as well.
On physical examination, there was a 12×10cm firm mass with an ill-defined margin in the lower inner quadrant of her right breast with tenderness and localized erythematous skin. Axillary lymph nodes were not palpable. She did not have nipple discharge. Her temperature and other vital signs were normal.
Breast ultrasound revealed a focal area of swollen breast lobules consistent with inflammatory reaction in the lower inner portion of the right breast with moderate skin thickening (Figure 1). Mastitis in the right breast was suspected; therefore she was admitted to the hospital for parenteral antibiotics and nonsteroidal anti-inflammatory drugs (NSAIDs). Three days later, the patient’s condition had improved and inflammatory symptoms had decreased, however, there was no change in the size of the mass. To confirm the definite diagnosis of the mass, a tissue biopsy was done by core needle method. Tissue was sent for histology, gram stain, acid-fast bacilli (AFB) stain, periodic acid-schiff (PAS) stain, aerobic and anaerobic cultures. All stains and cultures were negative. The histopathological evaluation showed poorly-formed noncaseating granulomas with many multinucleated histiocytes along with epitheloid cells, lymphocytes, aggregates of neutrophils and some eosinophils, which were compatible with idiopathic granulomatous mastitis (Figure 2). Microabscess formation was noted. Her chest imaging was also normal. A few days later she developed a fistula with pus-like discharge at the core biopsy wound. Although she was given oral antibiotics, there was no improvement. As the pain increased at her right breast mass with an area of induration and erythema, she subsequently underwent surgical incision and drainage. About 20 ml of purulent discharge drained from the lesion. Both discharge and inflamed tissue were sent for routine stains and cultures but all results returned negative. She received postoperative parenteral antibiotics and wound dressing changes (twice daily) for one week. As a result, the surgical wound improved with good granulation tissue and minimal pus discharge and all inflammatory symptoms disappeared. After being discharged, she took oral antibiotics and visited the breast clinic once a day for wound cleansing and dressing changes.
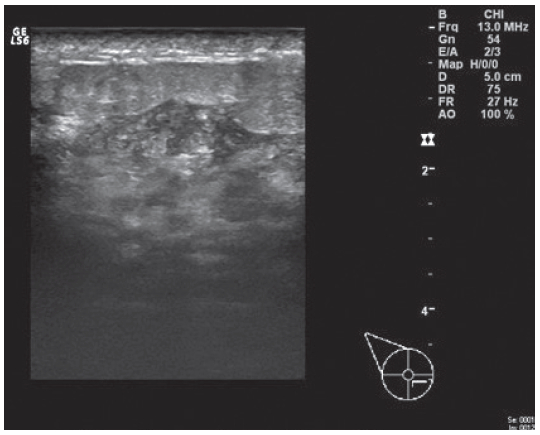
Figure 1: Ultrasonography of the patient’s right breast lesion. Focal inflammation with moderate skin thickening in the lower inner quadrant.
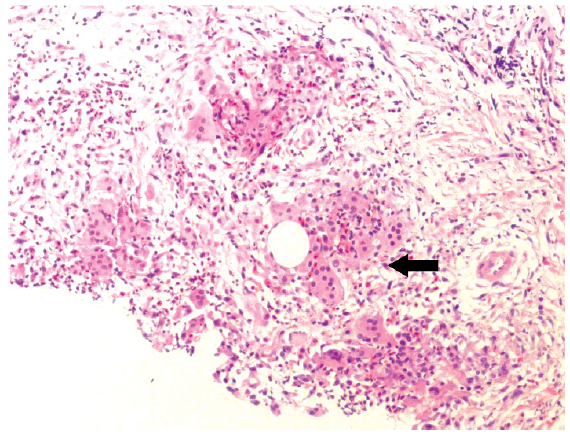
Figure 2: Histology slide of the patient’s right breast mass. Poorly-formed granulomas with multinucleated giant cells (Black arrow).
Two months later, the wound was completely healed and the size of the right breast mass had reduced slightly to 9.5 cm at its widest diameter. However, she developed a new painful 8.5×6 cm firm mass in the lower inner quadrant of the left breast with an ill-defined margin and signs of inflammation of the overlying skin like the previous one in her right breast (Figure 3). There was increased breast tissue density in the lower inner area of the left breast visible on the mammography. The ultrasound showed an ill-defined heterogeneous hypoechoic lesion at 8-9 o’clock of the left breast and surrounding tissue edema with skin thickening (Figure 4 and 5). The differential diagnoses were mastitis with early abscess formation, granuloma and inflammatory breast cancer. Initial treatment with NSAIDs had a good response. The inflammation had decreased and the left breast mass became about half the size. A core needle tissue biopsy was then performed for definitive diagnosis and the pathological report confirmed the diagnosis of idiopathic granulomatous mastitis. A week later, there was a fistula with minimal pus-like discharge at nipple areolar complex of the left breast near the mass area, while the core biopsy wound was well healed. A rheumatologist was consulted for evaluation and management of this case by using steroids. Several autoimmune serological tests were conducted, including anti-nuclear antibody (ANA), C-reactive protein, anti-double-stranded DNA antibody (anti-dsDNA), anti- Smith antibody (anti-Sm), anti-nuclear ribonucleoprotein antibody (anti-nRNP), anti-neutrophil cytoplasmic antibody (ANCA) and erythrocyte sedimentation rate (ESR) were ordered to rule out other autoimmune disorders and all tests provided negative results. The patient started on 20 mg of prednisolone daily and some improvement of symptoms was seen. The amount of discharge from one of the fistulas decreased and the size of both masses reduced significantly in just one week after starting this treatment. Three weeks later her symptoms had been completely resolved. The fistula closed and there was no palpable mass in both breasts. The patient maintained an initial dose of prednisolone for two months, then reduced this to 15 mg daily for four weeks and then to 5 mg daily over the next four weeks together with the addition of azathioprine at 50 mg daily.
After five months of treatment with steroids, prednisolone was tapered off completely. At the last follow-up visit, two months after stopping the steroid treatment, the patient was asymptomatic and no local recurrence was noted (Figure 6).
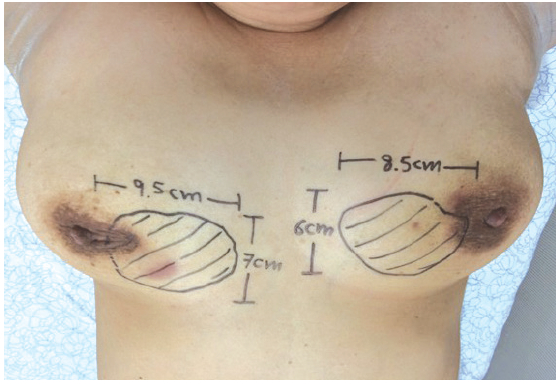
Figure 3: Clinical manifestation of bilateral breast masses of this patient diagnosed with bilateral idiopathic granulomatous mastitis.
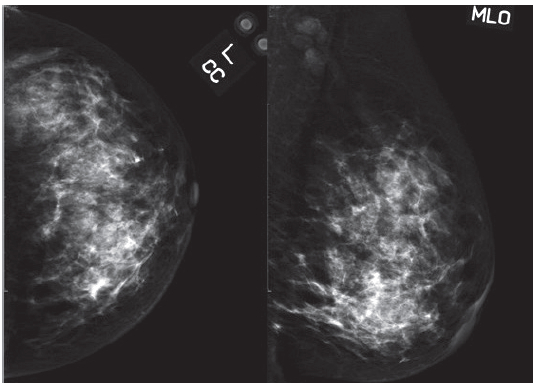
Figure 4: Mammography of the patient’s left breast lesion. Increased breast density in the lower inner quadrant.
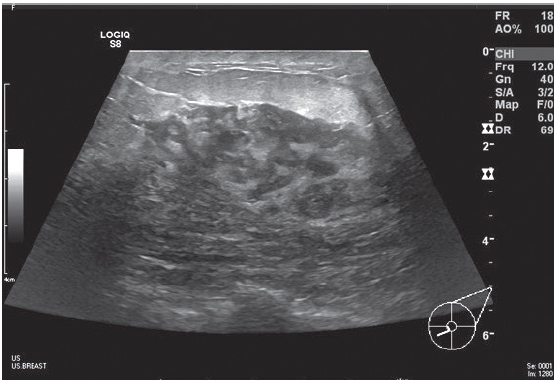
Figure 5: Ultrasonography of the patient’s left breast lesion. An ill-defined hypoechoic lesion in the lower inner quadrant.

Figure 6: The patient’s breasts at the last follow up visit after 5-months of steroid therapy.
Idiopathic granulomatous mastitis is a rarely seen, noncancerous, chronic inflammatory breast disease of unclear etiology and is diagnosed by exclusion.17 It’s commonly mistaken as common acute breast infection, infective mastitis or breast abscess and can clinically and radiologically imitate the symptoms of breast cancer, particularly if the regional lymph nodes are palpable.1,2,18 Misdiagnosis as carcinoma may result in unnecessary wide local excision or mastectomy.13,19 So a high index of suspicion is necessary. If symptoms of breast infection are not quickly improved or if there are repeated relapses after regular treatment, this disease should be included in the differential diagnosis.20,21
Idiopathic granulomatous mastitis is seen more commonly in young women of childbearing age and the usual age range is 22 to 42 years. However patients as young as 11 and as old as 83 years of age have been reported.5,8 Women with a history of pregnancy and breast lactation within the preceding five years are the most frequently affected.6 One third of the patients had previously used oral contraceptives.11,22 It is exceptionally rare in men and during pregnancy.23,24 Clinical presentation is usually unilateral, variable size, firm and ill-defined breast mass however bilateral lesions have also been reported in one fourth of cases.25 The mass can occur in any of the four quadrants of the breast except for the subareolar region.12,19 It is often associated with local tenderness, skin inflammation and nipple retraction like our patient with inflammatory mass in this report. In more chronic presen-tations, skin ulcerations, nipple inversion, fistulae and abscesses may eventually develop.3,10,13 Peau d’orange-like change of the overlying skin is rarely seen.7 While in some cases, no skin or nipple changes have been reported.26
The term granulomatous mastitis was first introduced by Veyssiere in 1967.27 Idiopathic granulomatous mastitis is defined as granulomatous mastitis without any evidence of infection and no specific causes. The exact etiology of this disease is currently unknown.19 Kessler and Wolloch who first described this disease in 1972 supported an autoimmune process corresponding to the histology.3 An association has been suggested with recent pregnancy and breastfeeding has led to the foreign body reaction to extravasated secretions from the breast lobules.28 Asso-ciations with blunt trauma, oral contraceptives, alpha-1-antitrypsin deficiency and hyperprolactinemia with galactorrhea (from pituitary prolactinoma or drug- induced galactorrhea) have also been reported.29,30
Mammographic features of this disease can be variable from normal findings in dense breast patients to masses with benign or malignant appearance and, most commonly focal asymmetrically increased density that mimic breast cancer. Sonographic imaging is also varied and relate to histologic patterns. The most common finding on breast ultrasonography is an irregular or ill-defined hypoechoic mass. Although breast MRI is better at detecting cancer than mammography and ultrasound it cannot differentiate between a granulomatous process and other inflammatory disorders.12,31
Histopathological evaluation remains the gold standard for the diagnosis of idiopathic granulomatous mastitis.7,12 This is because the clinical signs and radiologic findings of idiopathic granulomatous mastitis are indistinguishable from carcinoma of the breast especially inflammatory type.3,7,8,29,32 The differential diagnoses include carcinoma of the breast, other granulomatous breast infections such as tuberculous and mycotic infections especially when the fistulae to the skin occur, autoimmune diseases (sarcoidosis, Wegener’s granulomatosis), foreign body reaction and granulomatous reaction in cancer must be ruled out before diagnosing idiopathic granulomatous mastitis.19,25,32 A tissue sample is needed to avoid mis-diagnosing as breast cancer. The definitive diagnosis can be only made by tissue histopathological confirmation, so core needle tissue biopsy is preferred over fine needle aspiration cytology because a core biopsy is more accurate as it shows the tissue architecture.19 The microscopic features such as lobular non-caseating granulomas with epitheloid histiocytes, multinucleated giant cells and predominantly composed of inflammatory cells, mainly lymphocytes background, plasma cells and less frequent neutrophils with micro-abscess formation and no specific etiologic microorganism or agent favor diagnosis of this disease.7,12
The variable clinical course of idiopathic granulomatous mastitis is troublesome for both clinicians and patients particularly in recurrent cases. Because of the unclear etiology of the disease, an ideal treatment method has not been established. Treatment depends on the severity of the disease and may include expectant management, anti- biotics, steroids, other immunosuppressive drugs or surgical excision.9 The different rates of recurrence reported for each treatment method have been shown.2,4 Initial treatment should be non-operative and conservative treatment that is usually recommended in patients with mild symptoms or uncomplicated disease. Some studies reported that in close observation groups, spontaneous resolution seen in approximately half of cases without any treatment with a mean interval of complete resolution of 14.5 months (range 2 - 24 months).8
In most patients with idiopathic granulomatous mastitis the initial clinical presentation leads to the use of antibiotics. Antibiotics may be useful in the treatment of other granulomatous breast infection. But in true cases of idiopathic granulomatous mastitis, even an association with local infection with Corynebacterium species has recently been proposed33, antibiotics have no role in the management. This is because the condition of patients usually worsens or remains unresponsive to antibiotics and can lead to different antibiotic combinations.20,34
For patients with more severe symptoms, steroids are administered. Although a low-dose is preferred, steroids should be started at a dose of 1 mg/kg per day and continually higher doses administered until the lesions completely resolve, then taper the steroids slowly according to clinical response.21 Responses often present within weeks of treatment as seen in our patient. Treatment with steroids requires several months (usually up to six months) to achieve a complete response.5,21 Complete resolution of the disease is seen in 80% of those who received steroids.35 However about half of cases relapse after decreasing or stopping the dose of steroids.15,21 Longterm steroid use can produce many unpleasant and often permanent side effects, therefore rheumatologists should be asked to help in the management of these patients.27 The use of other immunosuppressive agents such as methotrexate or azathioprine as steroid-sparing drugs can be effective in treating patients refractory to steroid therapy, tapering steroid use and thus preventing many further complications after a long term treatment with steroids alone.4,15,27 Some studies reported that a good therapeutic response can be seen in patients treated with metho- trexate alone or in combination with steroids, with a more favorable side effect profile for treating idiopathic granulomatous mastitis.14 Colchicine and anti-inflammatory drugs (NSAIDs) have also been used and have proven efficacy.36,37
Finally surgical therapy as surgical excision and/or mastectomy should be considered in recurrent cases and cases unresponsive to conservative or medical treatment.13,38
Wide excision with negative margin is recommended due to a higher rate of recurrence after only a limited excision.12,36 For surgical treatment, recurrence rates of 5-50% have been reported and may be higher than steroid treatment in some studies.38 Furthermore, the high rate of postoperative wound complications and fistula formation have been reported.8 In other reports, surgical excisions were performed after medical treatment because preoperative steroid treatment provided significant regression of the inflammatory lesion and then allowed more conservative surgery.39
Idiopathic granulomatous mastitis is a rare, benign inflammatory breast disease that typically occurs in women of reproductive age. It is commonly mistaken for two common disorders, inflammatory breast cancer and infectious mastitis with abscess, so the definitive diagnosis is made using tissue histopathology. Only a high index of suspicion will prevent the morbidity of misdiagnosis or delayed diagnosis and inappropriate therapy. Treatment depends on the severity of symptoms and available treatment options include close follow-up, medical and surgical therapy. In the future if we know the clear etiology of this disease, a new potential treatment with low recurrence may yet be discovered.
Conflict of interests: The authors have declared no conflicts of interests.
Ethical approval: A written informed consent was obtained from the patient for publication of this case report.