Typical Clinical Scenarios
Case 1: A 15-year-old high functioning autistic boy with normal IQ was found to have episode of eyes rolling upwards followed by rhythmic body shaking and was unresponsive for 2 minutes. Ten hours after symptom onset, EEG study was performed and reported as normal . One week later, during playing soccer, he had another attack with similar pattern. Physical examination was unremarkable. Second EEG study was normal. He has no history of head injury. Family history was negative for seizure disorder. No developmental regression is mentioned. Should we prescribe antiepileptic drugs for this child?
Case 2: A 7-year 2-month-old autistic girl with severe develop- mental delays who has developed ‘bizarre behaviors’ described as head nodding and rapid eye blinking during listening to radio over a two week period. During sleep, she sometimes wakes up in the middle of the night and makes loud noises for 10 minutes before falling asleep again. These behaviors are unusual and have never occurred before. Regular medications included risperidone, methyl- phenidate, and zinc supplements. Are those ‘bizarre, unusual behaviors’ epilepsy or just stereotypic movements that are commonly found in autistic children?
Case 3: A 5-year-old autistic girl with epilepsy. Her seizures (generalized tonic-clonic) are well-controlled by valproic acid. She has had regular rehabilitation and physical therapy for motor and speech delay. Overall milestones are gradually improved. One day after being rebuked by a friend at school, she stopped speaking, not making any sound. However, she is able to follow verbal instruc- tion as usual. Parents are frightened and bring her to pediatrician for proper opinion. Has she developed language regression? Could this symptom be a subclinical seizure or just a behavioral reaction?
Case 4: A 10-year-old high functioning autistic boy is brought to clinic due to excessive drowsiness over two weeks. Actually his sleep duration is usually of 6-8 hours a day but has increased to 12-16 hours a day. Teachers have also reported to parents regard- ing his frequent falling asleep in the classroom. Normally, he is a good disciplined child and is always admired by parents, teachers and friends. Academic performance is average. He is a school tennis athlete. There is neither fever, history of head injury nor drug use during this episode. Physical examination is normal. Blood tests for CBC, electrolytes, sugar, BUN, Cr, liver function, thyroid function, and ammonia level are normal. CT scan of the brain shows negative study. Shall we consider ‘non-convulsive seizure’ as the cause of excessive sleepiness in this patient?
Outline:
1. Introduction of Autistic Spectrum Disorder (ASD)
2. Epilepsy in autism
2.1 Prevalence and risk factors
2.2 Types of seizures in autism
2.3 Subclinical epilepsy & autistic regression
2.4 EEG findings in autistic patients
3. Treatments of epilepsy in autism and autistic regression
4. Conclusion
Autistic spectrum disorder (ASD) is the umbrella term for life-long developmental disorders of brain in childhood comprising (1) autistic disorder or classic autism, (2) pervasive developmental disorder, not otherwise specified (PDD-NOS) or atypical autism,(3) Asperger’s disorder, (4) Rett’s disorder, and (5) childhood disintegrative disorder.1-2 The three core areas of malfunction of ASD are (i) impairments in social interaction, (ii) impairments in verbal and non- verbal communication and (iii) restricted, repetitive or stereotyped behaviors, interests and activities.3 The prev- alence of ASD is considered to be approximately 4 to 10 per 10,000 children from the 1980s and early 1990s, whereas recent studies have reported prevalence of 30 to 50 per 10,000 children.4 Highlighted on autistic disorder, the prevalence for classic autism representing the narrow phenotype is 0.1 – 0.3% and 0.3 – 0.6% for the broader ASDs.5 Clinical signs of ASD are frequently present at 3 years of age and recent prospective studies in toddlers indicate that abnormalities in social, communication and play behavior that may represent early indicators of autism can be detected as early as 14 months of age.6
Recent data indicate that the ‘autism epidemic’ is not real, and definitely not due to vaccines.7
Autism has a strong genetic basis and this neurode- velopmental disorder is the most clearly genetically influenced of all developmental disorders, including so-called ‘idiopathic autism’ without known etiology or comorbidity. A number of nuclear and mitochondrial genetic linkages have been identified – proof that differ- ent genes cause autism in unrelated affected individuals. Studies suggest that polygenic influences (i.e.multiple interacting genes) together with environmental/gene interactions are responsible for individual phenotypes.8, 9 In addition to genetic studies, recent work on the im- munology of autism suggests that there are specific serum antibodies in mothers of children with autism that recognize prenatally expressed brain antigen.10 Moreover, abnormalities of synaptic structure and brain function are at the forefront of current investigations of the brain basis of autism. The now well accepted alterations in cortical minicolumns with selective scarcity of gabaergic interneurons may be relevant to hyperexcitibility to sensory stimuli, increased seizure susceptibility, and systemic comorbidities in autism.11-13
Prevalence and risk factors
Epilepsy is defined as two unprovoked seizures of any type; therefore, febrile seizures (the most prevalent seizure of early childhood) and seizures in the course of acute trauma, infection, or metabolic illness are not classified as epilepsy. The prevalence of epilepsy among all children is estimated at 2 – 3%, compared with some 30% in autism.14 A bimodal age distribution of seizures is reported in autism. One peak occurs in infancy before age 5 years and the other in adolescence after age 10 years.15 The severity of cognitive impairment and the presence of cerebral palsy or other over motor deficits (Table 1) are the specific risk factors for epilepsy in children with ASD.16
Table 1: Cumulative probability of development of epilepsy in subgroups of children with autism as a function of age and severity of the underlying brain dysfunction16
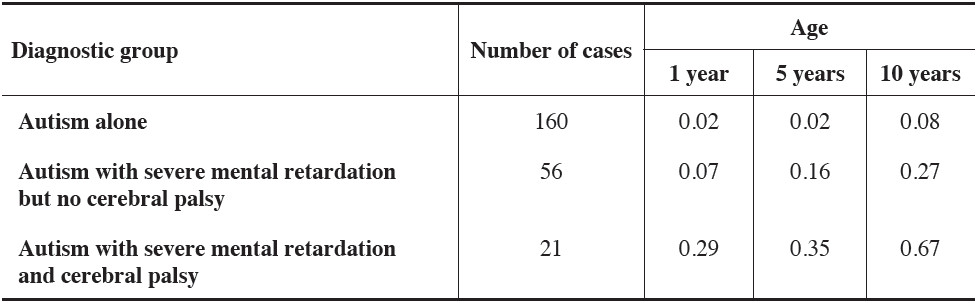
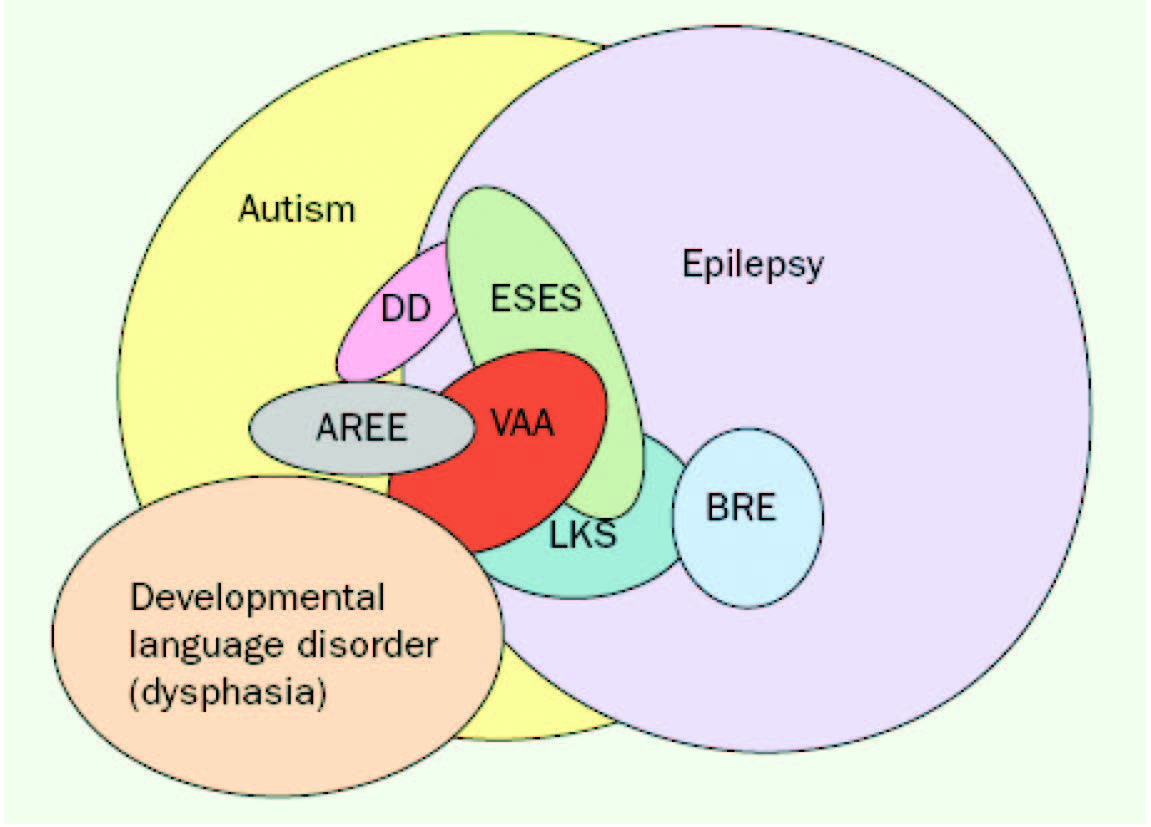
Figure 1: Overlaps between autism with or without epilepsy and other disorders of children with or with out language regression. Although an attempt has been made to suggest the relative prevalence of each disorder by the size of its oval, the sizes of the symbols and overlaps should not be taken literally because they were constrained by the need to show the multiple overlaps clearly (e.g., developmental language disorder should be larger, ESES smaller). AREE, autistic regression with an epileptiform EEG; BRE, benign rolandic epilepsy; DD, disintegrative disorder; VAA, verbal auditory agnosia.14
All seizure types can be associated with autism. The most prevalent seizure types found in a Swedish study were complex partial, atypical absence, myoclonic, and tonic-clonic seizures, whereas, generalized tonic-clonic and atypical absence seizures were the most common seizure type in a large American cohort.16, 17 Overt clinical seizures do not cause difficulty in diagnosis whereas subclinical, known as subtle or nonconvulsive, seizures may present with variety of under-recognized symptoms including complex, bizarre behaviors or unexplained deterioration level of consciousness. These symptoms could be underrecognized, particularly in autistic children with moderate-to-severe developmental delay. Subclinical epilepsy in this population are often overlooked and misdiagnosed. Moreover, until recently, more studies evidence the overlaps between autism with or without epilepsy as shown in Figure 1.
The clinical diagnosis of epilepsy in autism is com- plicated by the fact that subclinical complex absences may be mistaken for other childhood behaviors such as failing to respond to one’s name or to participate in an activity introduced by someone else. The unusual repetitive behaviors, such as tic-like movement, common in children with autism can be difficult to distinguish clinically from seizures. For clinicians faced with an autistic child who has no clinical convulsive seizures and an abnormal electroencephalogram (EEG), to prove a link between epilepsy and autism is difficult, especially if there is history of regression and the EEG is epilepti- form. Some studies suggest that epileptiform discharges on EEG without clinical seizures can cause behavioral and cognitive impairment.18, 19
In an open trial of valproic acid of 176 children with autism, 80 normalized on EEG and 30 more showed EEG improvement compared with the first EEG.20
This positive outcome offers hope that treatment of these subclinical abnormalities may act to prophylac- tically prevent future clinical seizure development. However, there is no current consensus on whether treatment of EEG abnormalities may influence develop- ment. Commencing anticonvulsant to autistic children with abnormal EEG, particularly in autistic regression, without clinical seizures is still debated and remains unanswered.
Children with autism may have normal EEG patterns that do give leave concern to parents and physicians. Conversely, abnormal EEG finding always raises questions to physicians, regarding definite diagnosis of epilepsy, especially for autistic children who do not have clinical seizures and those with regression.
Descriptions of EEG abnormalities have included not only epileptiform discharges (e.g. spikes, spike and wave, polyspikes, sharp wave discharges) but also less clearly abnormal features, such as “diffuse theta”, “low-voltage fast” and “amorphous background” which have been mentioned in many literatures. The fact is that the incidence of EEG abnormalities in nonepileptic children with autism has ranged from 6 to 83% but 46 to 59% with clinical seizures.20, 21 The EEG abnormali- ties include both generalized and focal abnormalities. The epileptiform activity is usually multifocal. Epilepsy is significantly more frequent in autistic youngsters with a history of regression compared with those without regression.22
The relation of clinical and subclinical epilepsy to autistic behavioral and language regression is intriguing but unresolved. Clinicians should consider investigating with EEGs, particularly children with history of regression, or fluctuations in language function, or new unfavorable behaviors. Several studies suggest that prolonged overnight EEG recordings have the highest yield to assess the presence of subclinical epileptiform activ- ity. Although there is controversy as to whether the epi- leptiform discharges are causally related to the language deficit or regression, the identification of such abnormal- ities offers possible therapeutic intervention.23
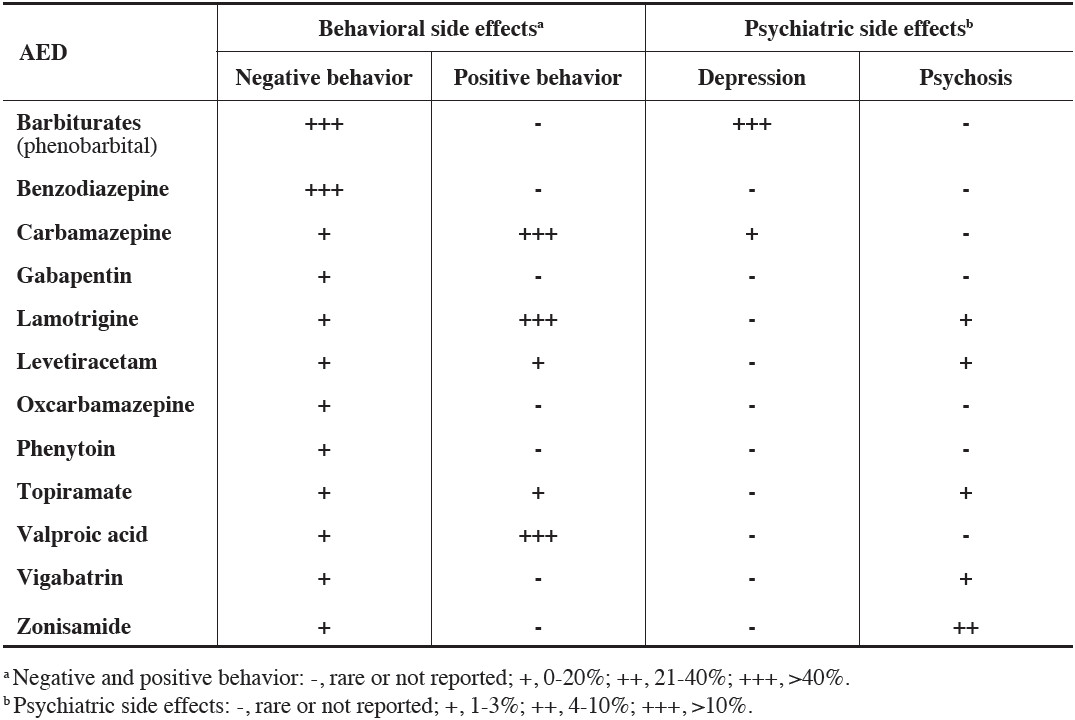
Table 2: General frequency of behavioral and psychiatric side effects of AEDs25
Medical treatment
The treatment of the seizures in autism is neither particularly difficult nor different from treatment of seizures in other children with epilepsy.24 Seizure types, EEG findings, and related illness history will guide neurolo- gist in choosing proper antiepileptic drug (AED). Crucial point of AED selection in autistic children is that clini- cian should avoid using medication that may aggravate seizure attack. Moreover, adverse effects of some AEDs causing negative behavior or psychiatric symptoms should also be considered.25 (Table 2) There are reports that the language of limited numbers of children with au- tism or autistic regression has improved in response to anticonvulsants, especially valproic acid, ethosuximide (not available in Thailand), and benzodiazepines.26 Im- provements have also been reported in patients treated with corticotrophin, steroids, or immunoglobulins.27-30
There are several clinical reports of the use of valproic acid in children with autism with or without clinical seizures but with epileptiform discharges on the EEG.20, 31-33 In an open trial of valproic acid, 10 of 14 individuals that completed the trial showed improvement in core symptoms and the associated affective instability, impulsivity, and aggression, and all patients with abnormal EEG or seizure history were rated as responders.34
Epilepsy surgery, such as surgical transection of epileptogenic foci, is mostly indicated to patients with intractable epilepsy. A few reports of children with autistic regression and clinical seizures revealed that epilepsy surgery affects positive outcomes for seizure control. Those studies hardly emphasized effectiveness of epilepsy surgery toward autistic symptom.35-37 One study stated that both language regression and behaviors were improved by using multiple subpial transections in 12 of 18 children with autistic regression, multifocal epileptiform EEGs, and subtle seizures (e.g. staring episodes, rapid eye blinking) without overt clinical seizures38 However, this study raises the question as to whether the use of such a potentially life-threatening intervention in autistic children who do not have intractable epilepsy is either medically logical and/or ethical. In summary, more systematic studies are required for developing guidelines of surgical treatment among autistic children either with or without clinical epilepsy.
Epilepsy in autism is not uncommon. The prevalence of epilepsy found in autistic children is up to 10 times higher compared with general pediatric population (30% vs. 2-3%). Autism and epilepsy co-occur in some genetic disorders that follow a Mendelian pattern of inheritance. These disorders may therefore share a common neu- rochemical substrate that is targeted by the psychotro- pic mechanism of action of several antiepileptic drugs. Diagnosis of epilepsy in autism is sometimes compli- cated. Convulsive seizures are not difficult to diagnose and clinicians may have no doubt to start antiepileptic drugs. In contrast, non-convulsive (or subclinical) seizure is under-recognized and this condition is often an overlooked diagnosis in children with autism. Autistic children with language regression or new peculiar behaviors cause more difficulty in diagnosis of epilepsy. Moreover, subtle symptoms such as inter- mittent eye blinking, tic-like symptoms or fluctuation of emotion may cause parents and clinicians to doubt whether those symptoms are indeed real seizures. In such scenarios, investigating with prolonged overnight EEG recording will provide the highest yield in detect- ing the presence of subclinical epileptiform discharges that may be causally related to language regression or other related symptoms. Despite there being no current consensus on whether treatment of EEG abnormalities may influence development, recent positive outcomes from copious clinical studies are more promising and offer possible therapeutic intervention, such as the option to use AED or corticosteroids. Adverse effect of some AEDs that might create adverse behavior or psychiatric symptom should be avoided.