http://www.new.bangkokmedjournal.com/article/storage/vol4/8/2-ab.jpg http://www.new.bangkokmedjournal.com/storage/vol4/8/1-ab.jpg
Arrhythmogenic right ventricular dysplasia (ARVD) is a type of nonischemic cardiomyopathy which primarily involves the right ventricle (RV). ARVD is considered a major cause of sudden death in young adults, mainly in the age group under thirty years old and is rarely found in the elderly. Males are predominantly affected.1-3 ARVD has been proposed as a genetic inherited disease with autosomal dominant and various penetrance patterns.4, 5 ARVD is pathologically characterized by fibro-fatty or fatty replacement of the right ventricular myocardial tissue. The fatty form is presented by almost complete replacement without endocardial thinning and found almost exclusively on the RV myocardium. The fibro-fatty replacement is defined as a fatty replacement with endocardial thinning less than 3 mm thickness6. The fibro-fatty replacement is considered a source of electrical instability of the RV in the form of ventricular arrhythmias with left bundle branch block morphology.2, 7 Many theories were proposed to explain the etiology and pathogenesis of ARVD such as apotosis or programmed cell death theory which leads to myocardial cell loss followed by fibro-fatty replacement and causes the RV increased vulnerability to life threatening arrhythmias.2 The most common triangle effected areas of the RV which are the sites of fatty and fibro-fatty replacement are the right ventricular inflow (sub-tricuspid area) and outflow tract including the RV apex.8 The fatty replacement can involve areas of the left ventricle (LV), the interventricular septum is spared in most cases. 9 The ARVD patient may present with a wide clinical spectrum, frequently asymptomatic with ectopic beat until sudden cardiac death. The typical clinical presentation is palpitation from ventricular arrhythmia, with left bundle branch block (LBBB) pattern which may be captured on electrocardiogram or holter monitoring.2, 10 Other typical electrocardiographic signs are the epsilon wave and prolonged QRS complex (>110 msec) with the absence of complete right bundle branch block (RBBB) in precordial lead V1-V3 of twelve -lead ECG. Because of wide range of clinical presentation of ARVD, the original criteria for ARVD diagnosis was proposed in the year 199411:
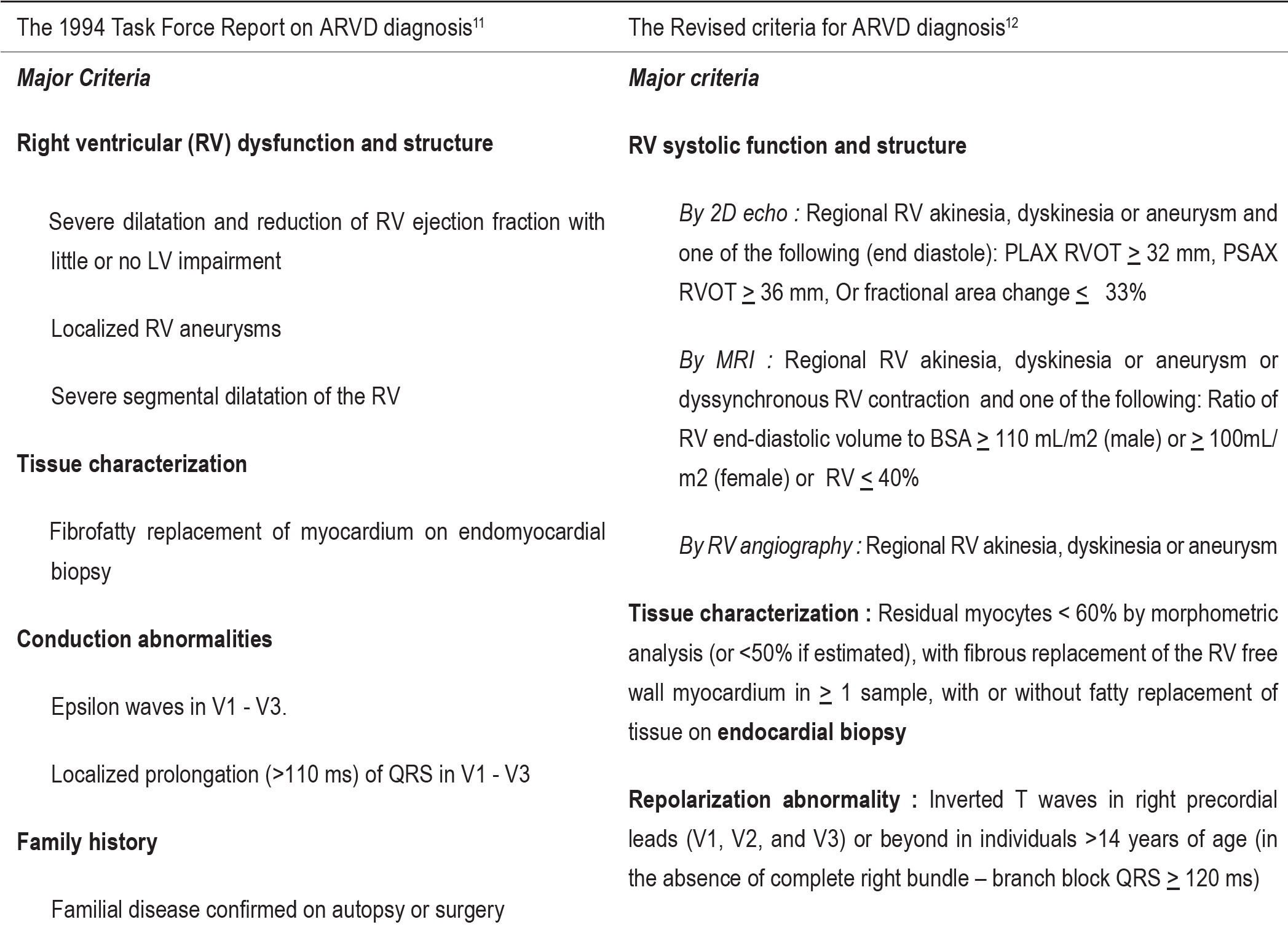
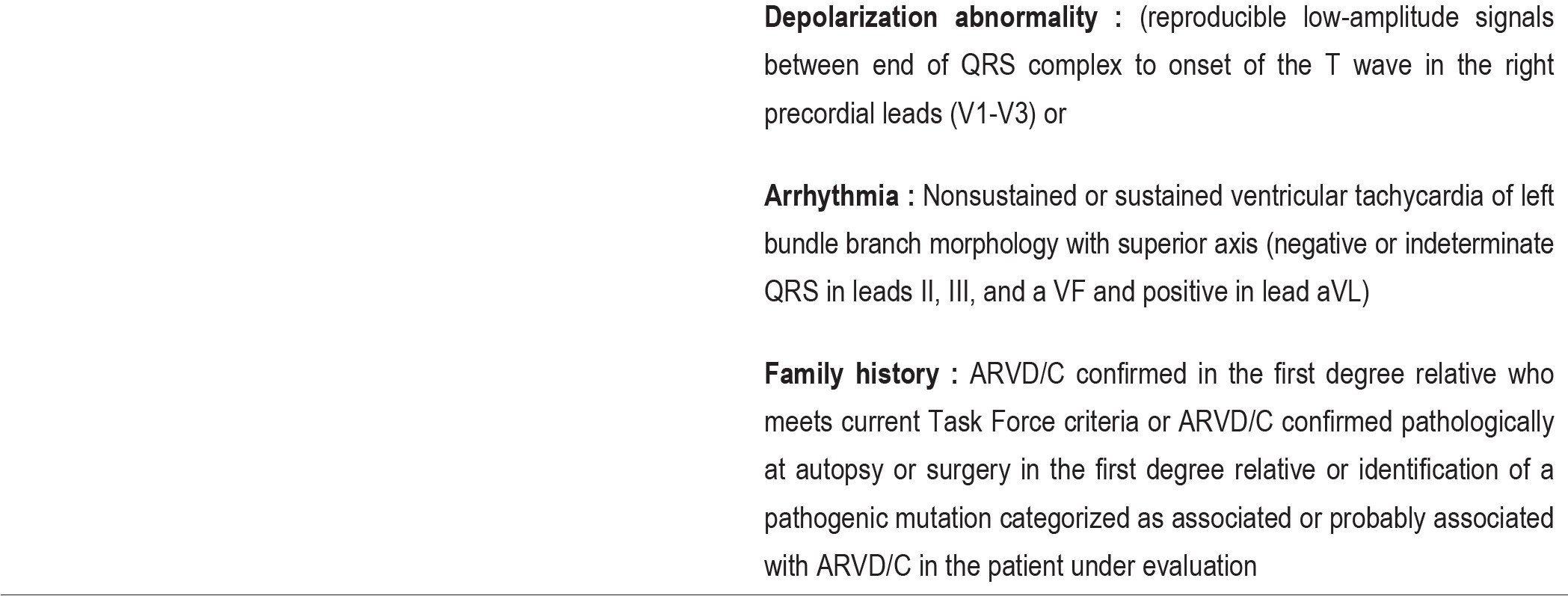
However, no single characteristic finding has been proved as a pathognomonic sign of ARVD. With regard to the original criteria, to diagnose ARVD requires either 2 major criteria or 1 major and 2 minor criteria or 4 minor criteria Table 1 below. Relying on the original diagnostic criteria for ARVD which was published and established in 1994 as shown, meant that ARVD would be diagnosed when the clinical conditions reach the overt stage therefore the early stage of ARVD would not be discovered. The new criteria for ARVD diagnosis was proposed in 2010 by Dr Frank Marcus and colleagues.12 This new criteria divided the possibility for being diagnosed an ARVD into three stages; Definite ARVD: 2 Major or 1 major and two minor or 4 minor criteria from different categories, Borderline ARVD: 1 major and 1 minor, 3 minor criteria from different categories, Possible ARVD: 1 major or 2 minor criteria from different categories. Some other characteristic findings were introduced to the revised criteria, to increase the diagnostic sensitivity
Table 1: The diagnostic criteria for ARVD
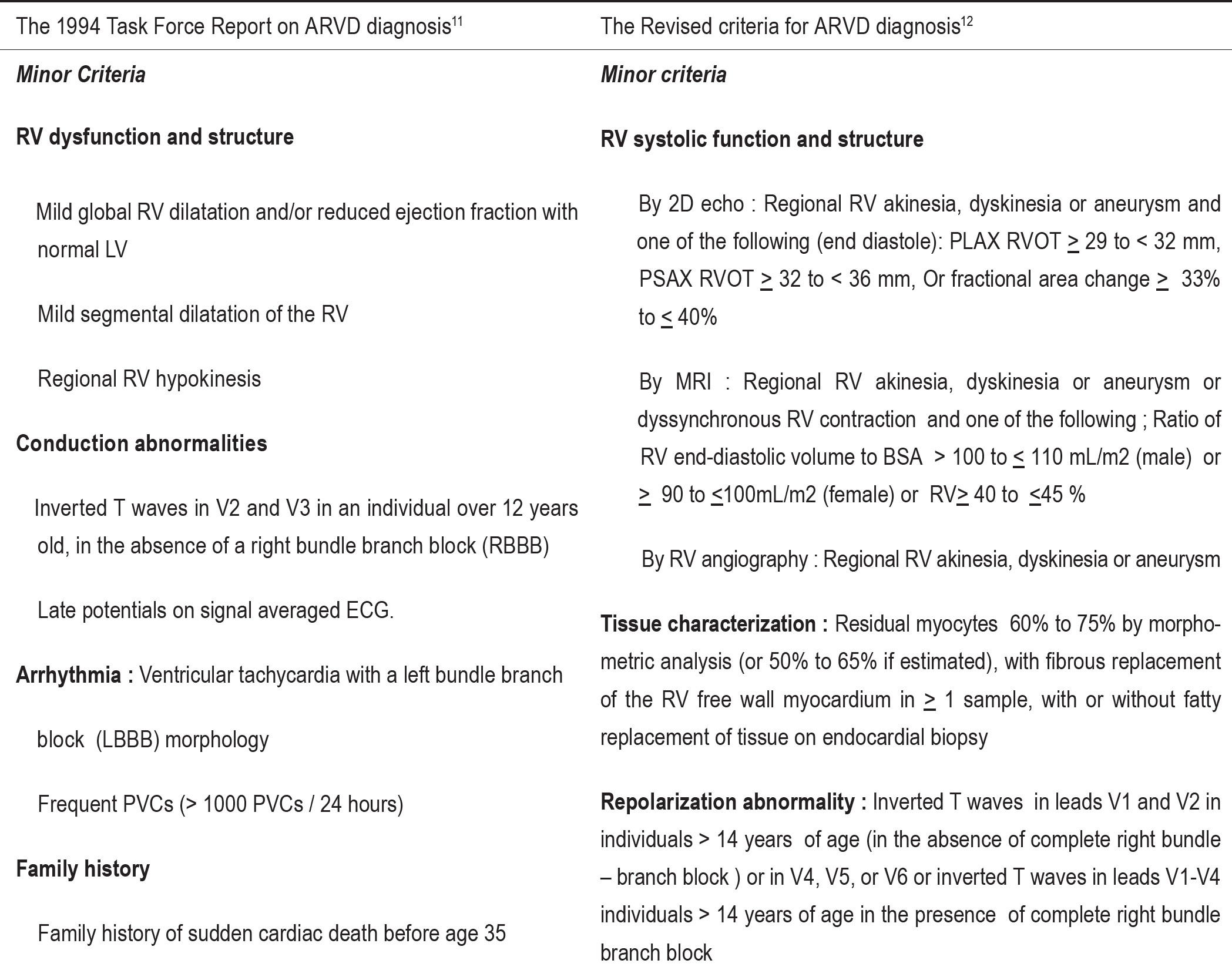
A 74-year-old Thai monk, with history of post endarterectomy of the left carotid artery, came to the hospital with vertigo and chronic fatigue. Physical examination was unremarkable. Twelve leads ECG revealed localized widening QRS wave of complete right bundle branch block in precordial lead V1 and widening of QRS complex with Osborn wave in precordial lead V2-V3 and no sign of ischemic change. Echocardiography revealed moderate RV systolic dysfunction (RVEF = 45.0%) with moderate hypokinesia of the RV apex. Multi-slice Computed Tomography for coronary artery revealed normal study. The patient was sent to MRI center for cardiac MRI to find out the cause of right ventricular dysfunction. Cardiac MRI with gradient echo CINE technique revealed normal size of the RV and hypokinesia of the right ventricular apex on horizontal long axis view images. Fatty replacement in right ventricular myocardial tissue was demonstrated on the T1W black blood MRI images which is compatible with the result of cardiac MRI by spin echo T2W BB with fat suppression technique. By delayed contrast (gadolinium) enhancement MRI study, myocardial contrast enhancement of both ventricles was not demonstrated. This patient was diagnosed as a borderline ARVD by the result of MRI examination met one major criterion and one minor criterion of ARVD diagnosis in different categories according to the original criteria.
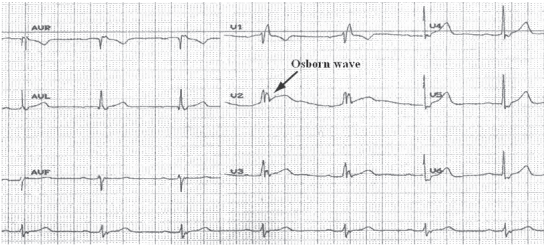
Figure 1: Demonstration of widening QRS complex of complete right bundle branch block in lead V1, widening QRS complex with Osborn wave in lead V2-V3
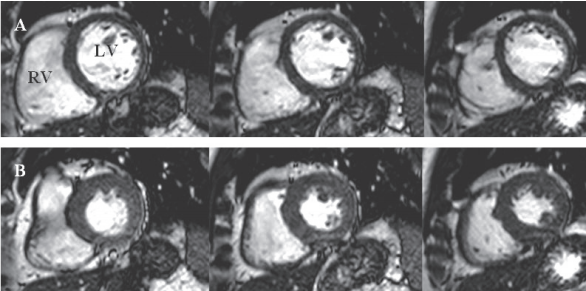
Figure 2: Gradient echo CINE MRI images on short axis view reveal moderate RV systolic function with mild global hypokinesia (RVEF = 45.0%, normal = 54-78%). Series A: diastolic phase; Series B: systolic phase
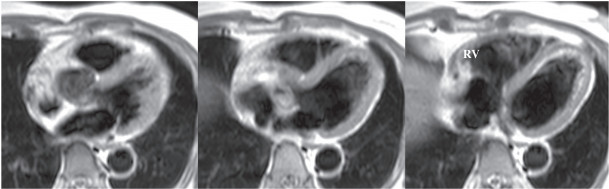
Figure 3: T1W black blood MRI images reveal fibro-fatty replacement (myocardial tissue = gray intensity, fatty = white band) at the RV apex (in box)
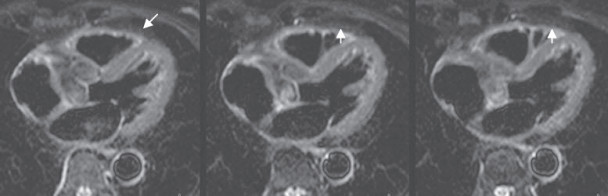
Figure 4: T2W black blood fat suppression MRI reveal hypointensity of fat which replaced RV myocardium tissue (gray intensity, white arrow) which was compatible with the white band of fatty replacement as shown on T1W black blood images
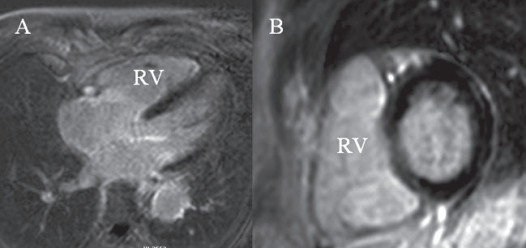
Figure 5: MRI with Delayed contrast enhancement technique revealed no myocardial contrast enhancement of the left ventricle and right ventricle. A: Horizontal long axis view, B: short axis view of both ventricles
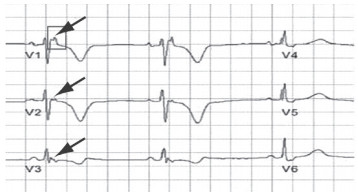
Figure 6: Demonstration of the epsilon wave character in precordial lead V1-V3 (arrow)
1. Case report
In this article, we describe a borderline ARVD in an elderly patient older than 65 years. The clinical signs of the patient obtained from CMRI met one major criteria of tissue characterization as fatty replacement in the RV myocardial tissue and one minor criteria of RV dysfunction with apical RV hypokinesia regarding to the original criteria (1994). Although ARVD is considered a disease of young adult with mean age less than 30 years and rarely occurs in the elderly (more than 65 years)13, however, to diagnose ARVD in both young adult and elderly groups follows the same criteria. Therefore, ARVD should be considered individually in line with supporting evidences. The typical clinical presentations are often palpitation from ventricular arrhythmia or near syncope or even sudden cardiac death. ARVD should be taken into account in case of ventricular arrhythmia of the right heart without other overt myocardial diseases. The electrocardiographic signs of our patient were CRBBB with T wave inversion in precordial lead V1 and widening QRS complex with Osborn wave in precordial lead V2-V3, which were not matched for the typical characteristic findings of the ARVD. Osborn waves were positive deflections occurring at the junction between the QRS complex and the ST segment where the S point, also known as the J point, has a myocardial infarction-like elevation [These waves were described in 1953 by JJ Osborn]. Osborn wave is often found in case of hypotemperature (< 32 °C), hypercalcemia, brain injury, vasospastic angina or ventricular fibrillation14. Epsilon wave which is one of the typical sign of the ARVD and is found about 33% in ARVD patient (Khurram N et al15 2004). This is described as a terminal notch in the QRS complex. The epsilon wave is more often seen on signal averaged ECGs and occasionally observed on twelve lead ECG. The electrocardiographic sign of right bundle branch block was found in around 17% of ARVD cases (Jain R et al.16 2009). Complete right bundle branch block (CRBBB) on precordial lead has been introduced into the minor subgroup of revised criteria (2010) as a character of CRBBB with T wave inversion on precordial lead V1-V4 but T wave inversion on precordial lead V1-V3 without CRBBB is classified as a characteristic finding in major subgroup of abnormal repolarization abnormality regarding to both original and revised criteria for ARVD diagnosis. Normally, this character may be seen in less than 3% in normal healthy heart.17, 21 Although ARVD is characterized by the fatty replacement in the RV myocardium but it is not the hallmark of ARVD. Fatty replacement in the RV myocardium is classified as one only of the characteristic findings of major criteria for ARVD diagnosis. Significant fatty infiltration of the RV is observed in more than 50% of normal heart in elderly people18 but in typical cases with presence of VT with LBBB pattern a high percentage of fatty replacement is not found.19 Fatty and fibro-fatty replacement in the RV myocardial tissue can be characterized by using MRI and endomyocardial biopsy. MRI is a good alternative modality for RV tissue characterization. The sensitivity of the use of spin echo T1W bb MRI for characterization of the fatty replacement was not high (67%) and the specificity was of 100%18 hence the presence of fatty replacement of the RV myocardium should be considered as a diagnostic factor when using with other indicative clinical characters for ARVD diagnosis and the absence of fatty replacement in the RV myocardium in highly suspicious cases does not rule out ARVD.
2. MRI and ARVD assessment
Imaging techniques for ARVD assessment include echocardiography, conventional RV angiography and Magnetic Resonance Imaging. Echocardiography and RV angiography are very good at RV structure and function assessment but these imaging techniques have the limitation of spatial resolution to characterize the typical fatty and fibro-fatty replacement of the RV myocardium. Only Magnetic resonance imaging (MRI) is a promising tool for evaluation anatomy and function of the right ventricle and is frequently used to characterize fatty replacement on the RV myocardial wall.20,21 ARVD diagnosis frequency has demonstrably increased since MRI became established in use for ARVD diagnosis.22 MRI can demonstrate the typical characters which are proposed in both major and minor criteria in terms of RV systolic dysfunction and structural changes including RV myocardial tissue characterization. Gradient echo CINE MRI technique is used to demonstrate the RV structure and to assess the RV systolic function. RV systolic function assessment was done by using semi-manual delineation of the endocardial lining of the RV in every slice from basal to the apex (on short axis view of Gradient echo CINE MRI images) of in both diastole and systole. The RV ejection fraction was calculated by computerized program on the work station. Some special MRI techniques are used for ARVD diagnosis. The spin echo T1W BB MRI technique is used to characterize the fatty replacement on the RV myocardial tissue. The fatty replacement on the RV myocardial tissue is presented as hyperintensity signal tissue band with irregular demarcation on the intermediate intensity signal RV myocardial tissue. The spin echo T2W bb MRI with fat suppression technique may be used to confirm the result of ordinary T1W bb MRI by producing of the hypointensity signal of fatty replacement which is compatible with the hyperintensity signal of fat which is seen on the ordinary T1W bb images. Delayed contrast enhancement study MRI is used to detect myocardial fibrosis in both right and left ventricular myocardium. Although MRI has proved to permit myocardial fibrosis characterization in the left ventricle, however it may also produce uncertain results in the RV because RV has thinning myocardium and may be confusing with fat signal20,23 and may be missed due to very small area of fibrosis. To document fatty replacement on the RV myocardial tissue on MRI image, eye visualization methods are used, therefore varying experience among the interpreters may cause uncertain accuracy in ARVD diagnosis using MRI.
3. Diagnostic criteria
Although the original 1994 criteria are too rigid to detect the early stages of ARVD yet it allows the true typical case to be detected with very high accuracy. The revised 2010 criteria were created with improved sensitivity and preserved specificity, aiming for early evaluation the non-overt stage group. As regards the original criteria, MRI was allowed as a tool for fatty or fibro fatty replacement characterization but it is not for the revised criteria. As a matter of fact. the standard of reference for the diagnosis ARVD is based on histologic demonstration of fatty or fibro-fatty replacement of the RV myocardium by autopsy or surgery. However, endomyocardial biopsy which is used for tissue characterization according to the revised criteria lacks sufficient sensitivity to diagnose ARVD because of sampling errors.22 Therefore, to confirm diagnosis by endomyocardial biopsy is not recommended. For assessing the development of disease in the first relatives of patients with ARVD, non-invasive testing should be taken into consideration as an alternative following the revised criteria.
No single criterion has been proved to be used alone for ARVD diagnosis because ARVD has various clinical presenting signs. Diagnosis ARVD in both young adult and elderly use the same diagnostic criteria. To assess the risk of the first relative of ARVD patient can follow the revised criteria using noninvasive test. Ventricular arrhythmia with left bundle branch block pattern, fatty or fibro-fatty replacement and RV systolic dysfunction with regional aneurysm are the typical characters which are often found in true ARVD case. Positive MRI finding of fatty replacement in RV myocardium can be found in normal healthy heart and, in the opposite, negative MRI findings of fatty replacement in highly suspicious case does not rule out ARVD. RV disorder conditions such as myocarditis or sarcoidosis which may present clinical features which mimic ARVC must be excluded in suspicious ARVD cases. Although CMRI is the tool that provides the most important anatomic, functional and histologic clues for ARVD diagnosis within a single study, the degree of variability among the MRI interpreters may, as aforementioned, be related in part to their experience with CMR diagnosis of ARVD, especially in fatty replacement characterization and identification.