A cognitive function (i.e. when an ADL is performed independently), for any patient who is terminally ill, uncontrolled after, and two prospective randomized trials had reported a favorable outcome of comatose survivors of out-of- hospital cardiac arrest when comparing mild hypothermia with normothermia in 20021,2 with many other studies published thereafter to support the benefits of therapeutic hypothermia in many different scenarios.3-5 Therapeutic hypothermia is now a standard approach in the care of comatose post cardiac arrest patients, and was recommended by the International Liaison Committee on Resuscitation in 20036 and the American Heart Association in 2010.1 Our hospital is a 517 beds hospital with 105 intensive care unit (ICU) beds with a 24 hours Cath lab. In 2013, we set up a therapeutic hypothermia working group including a medical transport team, a neurologist, an intensivist and a cardiologist. Our protocol includes all comatose post cardiac arrest patients (under 12 hours after return of spontaneous circulation (ROSC)) with previous good bleeding or arrhythmia, multiple organ damage; a patient who has opted for do not attempt resuscitation (DNAR), is excluded. Three cases were transferred to our hospital after cooling had begun at the referring hospital.
A 48-year-old male suffered a cardiac arrest at home. His wife woke up after she heard a gasping sound from the patient. She then called the local ambulance service and gave cardiopulmonary resuscitation (CPR). Fifteen minutes later upon the arrival of the emergency medical services (EMS) the monitor revealed ventricular fibrillation; after 3 shocks were delivered and a further 10 minutes CPR at the scene, the patient developed ROSC during transportation to a medical facility. After ROSC, the patient was comatose with a Glasgow coma score (GCS) of 6-T (E2M3VT), and the brain CT scan showed a mild degree of brain edema. The patient was then moved to the ICU and therapeutic hypothermia was started 2 hours after ROSC using a cooling blanket. During the cooling process, the patient was sedated and paralyzed. His core temperature was measured by an esophageal probe and the target temperature of 33 °C was achieved 3 hours later. A cardiac cause was highly suspected despite a normal electrocardiogram (ECG). After an hour of cooling, enoxaparin was administered and the decision was made for medical transportation to undergo further investigation and management including cardiac catheteri- zation. The estimated ground transport time was six hours round trip, and the time from the ICU (at referring hospital) to the ambulance parking area was 5 minutes. After discussions with the patient’s family and the transport team, we immediately dispatched a mobile cardiac care unit with 1 cardiologist, 2 emergency nurses,1 emergency medical technician-basic (EMT-B) and 1 porter. The transportation plan was made under the supervision of medical control. Given the requirement of an additional power supply required for the Arctic Sun 2000® surface cooling system on the ambulance, the team was advised before departure to ensure there was a fully operational internal battery on board. This would power all other equipment including the ventilator, monitor, defibrillator, infusion pump and suction. The plan was that upon arrival the Arctic Sun 2000® would be turned on in the ambulance whilst the esophageal temperature probe and hypothermia pad were being applied at the referring ICU before moving the patient. At the referring hospital’s ICU, the patient’s core temperature was 34 °C and his GCS was 3-T (E1M1VT) under sedation and paralysis. After 5 minutes of moving from the ICU to the ambulance without cooling, the core temperature measured by the Arctic Sun 2000® on the ambulance was 34.2 °C. During transportation the patient’s core temperature was under control (Figure 1) and his vital signs remained stable. He was cooled for 24 hours and rewarmed for 20 hours. During hospital admission his hemodynamic was stable without inotropic agent and the initial ECG was normal. Fifty hours after ROSC (4 hours after the patient came off sedation and paralytic drugs) the patient was fully alert and he was then extubated 10 hours later. The complication during hypothermia was a mild upper gastrointestinal hemorrhage (coffee ground content in the nasogastric tube). Potassium levels were initially low (3.3 mmol/L) during the cooling induction. At 24 hours, the EEG monitoring revealed no epileptiform activity. On day three, a coronary angiogram was done and revealed 10-20% stenosis at the mid left anterior descending (LAD). After waking, the patient reported a history of sudden cardiac death in his family. With a suspicion of Brugada syndrome, a cardiac electrophysiologist was consulted and an automatic implantable cardioverter defibrillator (AICD) application was advised to the patient and his family. He was discharged home six days after admission with cerebral performance category (CPC) 1 without neurological deficit.
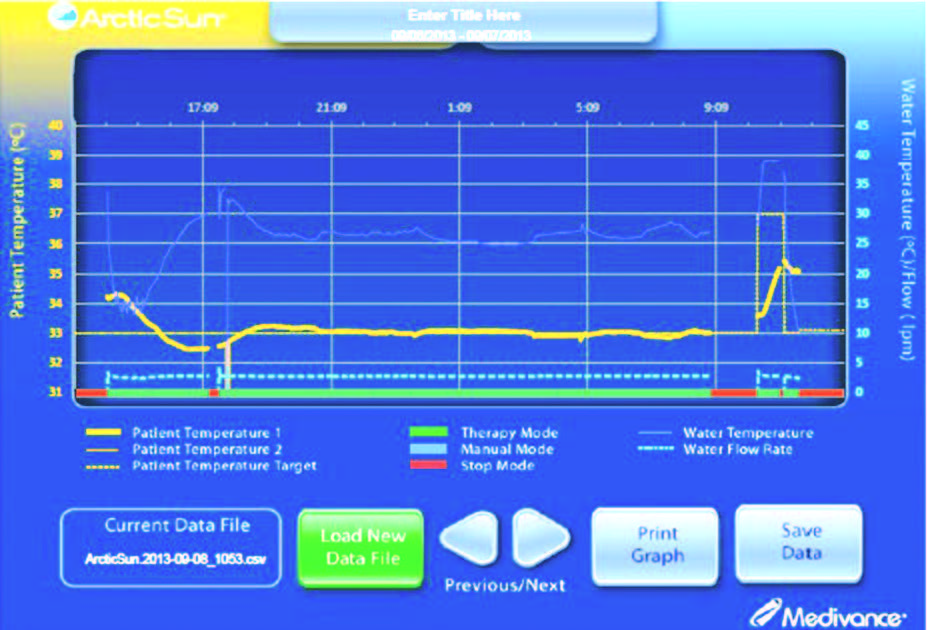
Figure 1: Patient’s temperature during ground transportation.
A 47-year-old male suddenly collapsed and was transported by local EMS without CPR. Twenty minutes after collapse he arrived at the local emergency department and CPR was immediately started. The initial rhythm was ventricular fibrillation. After 23 minutes of CPR with defibrillation performed four times, the patient developed ROSC. After ROSC his GCS was 3-T and the ECG showed ST elevation in V2-V3, and a thrombolytic was administered at the local hospital. The patient was then transferred to the provincial hospital, cooled with saline and icepacks. At the provincial hospital, a coronary angiogram was performed with a negative result, and therapeutic hypothermia continued with a cooling blanket and monitoring of core temperature with an esophageal temperature probe. The target core temperature of 33 °C was achieved at 5 hours after ROSC. The patient was administered a Dopamine and Norepinephrine intravenous (IV) drip to control blood pressure. The transport team was then alerted. The estimated ground transport time was 18 hours round trip. After discussions with the patient’s family, a transport team with a fixed wing aircraft was dispatched. As the target temperature machine was not available at that time, the local hospital was requested to prepare cooled IV saline solution and icepacks and a repeat of blood electrolytes. Hypokalemia had been reported and was corrected before the transport team arrived. At the referring hospital’s ICU, the patient’s core temperature was 34 °C and his vital signs were stable. During transportation, the patient was cooled with cool IV saline and icepacks. Temperature was measured at the axilla with a temperature between 34 °C to 34.8 °C (a core temperature monitor was not available at that time) and his vital signs remained stable. The total transport time was three hours (ground and air transport). On arrival to the cardiac care unit, his core temperature measured by esophageal probe was 34 °C and cooling was then started with the Gaymar Medi-Therm III 7900 external cooling system. The brain CT scan before cooling revealed a brain edema. After 24 hours of cooling and 20 hours rewarming, sedation and paralysis was discontinued. He remained comatose for 27 days and was extubated 38 days after admission. On the first day of admission he developed seizures; an antiepileptic drug was administered by a neurologist. The EEG monitoring revealed mild encepha- lopathy without epileptiform activity. Five days after admission he developed stormed ventricular fibrillation which was refractory to medication. A stellate ganglion block was performed with a partial response. He was eventually put on AICD 18 days later. He had also developed acute renal failure and required hemodialysis for a month when his kidney function was then fully recovered. Another complication was rectal laceration with massive bleeding and pneumonia. Two months post cardiac arrest, the patient is now in rehabilitation with CPC 1.
A 50-year-old male with underlying dyslipidemia was brought to a private hospital in Chiangmai province with sudden cardiac arrest. After a day of ongoing chest pain, the patient was transported to the hospital by his family. During transportation, he suddenly collapsed in the car and was given CPR by his family. Ten minutes later, the patient arrived at the emergency department, the initial rhythm was ventricular fibrillation. CPR was continued for 12 minutes before ROSC. After ROSC he was comatose with GCS 3-T, his ECG revealed ST segment elevation in V2-V6. He was immediately sent to the Cath lab for primary percutaneous intervention (PCI) which revealed total proximal LAD occlusion. PCI was successfully done. He was then transferred to the ICU and started therapeutic hypothermia at 2 hours after ROSC. The target core temperature of 33 °C was achieved 4 hours later. The brain CT scan was normal and the EEG revealed moderate encephalopathy with no epileptiform discharge. After 20 hours of cooling, air transportation to our hospital was requested. The Arctic Sun 2000® was placed on the aircraft and was transported to the referring hospital. On arrival at the referring hospital’s ICU, the patient’s temperature was noted to be 33 °C. A cooling pad was attached and an esophageal temperature probe was inserted at the ICU before moving the patient to the ambulance. He was cooled with The Arctic Sun 2000® surface cooling during ground and air transport. The total transport time was 3 hours. His vital signs remained stable without inotrope. After arriving at the ICU, rewarming was then initiated. The patient had been totally cool for 29 hours and rewarmed for 20 hours. He was fully alert six days later and was extubated two weeks after the cardiac arrest. He was discharged from the hospital three weeks later with CPC 1.
The use of therapeutic hypothermia in post cardiac arrest care has risen around the world as well as in Thailand. Beside hypothermia, systematic post cardiac arrest care is considered an important factor in improving survival rates and reducing morbidity. Post cardiac arrest care requires multiple investigations, interventions and the inputs of several specialists (i.e. an intensivist, a cardiologist, a cardiac interventionist, and a neurologist). This has increased the need to transfer of care from local facilities to more well equipped tertiary health care institutions. Successful active cooling during transportation had been previously reported in neonatal cases with hypoxic ischemic encephalopathy.7 A good co-ordination of efforts between the referring hospital, the transport team and the receiving facility is key to the success of every case of medical evacuation. With a limited number of target temperature machines (TTM) available, passive cooling with ice pack and cool saline has been used. This may result in under or overcooled patients and peripheral temperature is normally unreliable in mild hypothermia. Temperature monitoring with an installed core temperature will be useful in cases where the TTM is not available or other cooling methods are used such as EMCOOLS Flex.PadTM. Recently, a few studies support the accuracy of tympanic temperature during therapeutic hypothermia which may prove useful as an alternate tool.8,9 The TTM is ideally the most accurate cooling method and has decreased the burden on patient care especially post cardiac arrest patients who are normally on ventilators and require multiple drug administration.10,11 Similarly to other target temperature machines, using the Arctic Sun 2000® surface cooling during transportation has some considered limitations. Without a back-up battery, The Arctic Sun 2000® surface cooling needs to be plugged in at all times. Using the direct power supply from an ambulance diverter can result in a power shortage. A fully charged back-up battery should be made available to ensure an adequate power supply for all equipment during transportation (e.g. ventilator, monitor, defibrillator and suction). While transporting the patient without TTM (i.e. transferring from ward to ambulance or from ambulance to aircraft), passive cooling with icepacks or cool saline can be applied with a continuous monitoring of core temperature (if the transfer period is long) to minimize temperature fluctuation.7 The Arctic Sun 2000® surface cooling weighs 47 kilograms (103 lbs) when filled with water, therefore the team should ensure sufficient-manpower to move and install the machine. Safety is a concern when there is no installed mounting arrangement in the ambulance or aircraft for this equipment.
In summary, in the case of post cardiac arrest patients, we recommend the development of a transportation protocol for the timely activation of therapeutic hypothermia and the early transportation to an appropriate facility. Pre-planned transportation procedures should also be written and the power supply of the transport vehicle should be regularly tested and checked. Using TTM during transportation is highly recommended. Where TTM is not available, alternative cooling methods such as icepack and cool saline can be used. This should be coupled with esophageal, rectal or bladder temperature measurements with a standard multi-monitor, although tympanic temperature measurement is another option. Furthermore, the target temperature machine should have a back-up battery. Finally, a standard, secured mounting for the machine is required to ensure safety during transportation.