Aberrant right subclavian artery (ARSA), also called arteria lusoria, is one of the most common intrathoracic arterial anomalies. Although most of the patients are asymptomatic the retroesophageal and retrotracheal course of the lusorian artery might result in non-specific chest pain, dysphagia, dyspnea, arterioesophageal or arteriotracheal fistula with hematemesis or hemoptysis, and aneurysmal formation with relevant risk of rupture. The first case report of dysphagia from ARSA was reported by David Bayford in 1794.1 The prevalence of this rare congenital anomaly is around 0.5-2%.2 Normally the right subclavian artery (RSA) develops from the fusion of the persistent right proximal dorsal aorta with the right seventh intersegmental artery distally. The abnormal origin of the RSA is caused by the involution of the right fourth vascular arch and proximal right dorsal aorta and the persistence of the seventh intersegmental artery originating from the proximal descending thoracic aorta, forming the aberrant course of the lusorian artery.3 The arteria lusoria arises from an aortic arch diverticulum at the proximal descending aorta, first described by Kommerell.4 According to variables of underlying vascular pathology, various surgical procedures were chosen for appropriate cases. The operative procedures could be done via median sternotomy, supraclavicular approach, and transaxillary thoracotomy approach, with or without heart-lung machine support. Recently, endovascular surgery has been chosen as an alternative procedure in some cases.5,6
A 73-year-old female patient had clinical symptoms of dysphagia in association with an ARSA; her body weight dropped from 60kg to 31kg in 6 months. She also had symptoms of broncospasm from time to time and needed broncodilators for treatment. The chest radiography showed a prominent aortic knob (Figure 1).
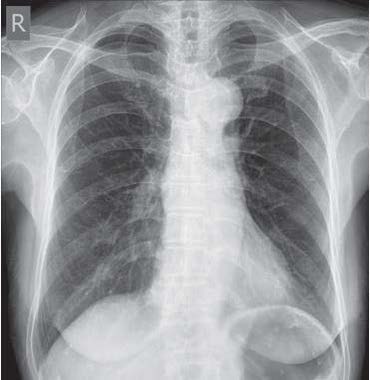
Figure 1: Chest x-ray on pre-operative day.
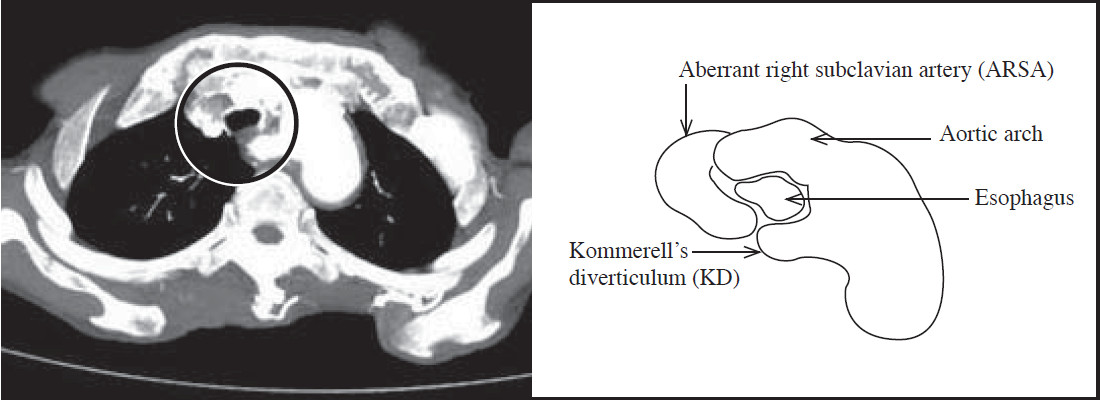
Figure 2: The computer tomography shows the esophagus being trapped between Kommerell’s diverticulum (KD) and the trachea (in the circle).
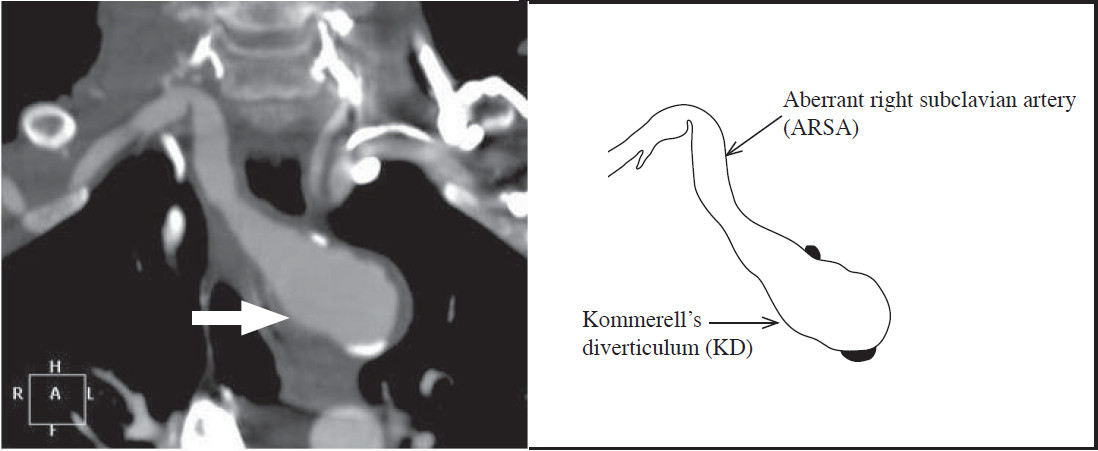
Figure 3: The computer tomography shows Kommerell’s diverticulum (KD) (white arrow).
The computer tomography showed the ARSA with Kommerell diverticulum (KD) compressing the esophagus (Figure 2-4). An open surgery and endovascular procedure were proposed to the patient’s family as options and they chose the open surgery option.
The patient was prepared under general anesthesic and put in a left lateral decubitus position and bilateral radial artery monitoring was performed. The right transaxillary approach was undertaken via the 3rd intercostal space. The ARSA was mobilized and divided; both ends of the artery were closed with No.4-0 polypropylene suture and reinforced with pledgeted (Figure 5). The esophagus was moved away from the surrounding tissue. The right radial mean arterial pressure was 45 mmHg, while the right index pulse oxygenation was around 70%. The reanastomosis of the right subclavian artery was abandoned. A No. 28 drainage tube was inserted in the right pleural space. The patient was extubated immediately post operation. The oxygen saturation on the right hand increased to 95%, while the mean arterial pressure was around 70 mmHg, with a normal wave form.
The patient had a liquid diet on postoperative day 1 and a soft diet on day 3. The intercostal drainage tube was removed. She was discharged home on postoperative day 7. She gained around 3kg in weight in the first month after being discharged and had only one episode of a mild broncospasm attack. She resumed her normal daily activities in the 2nd month after surgery, without clinical signs of broncospasm. By the 3 months follow-up, the patient had gained a further 3kg.
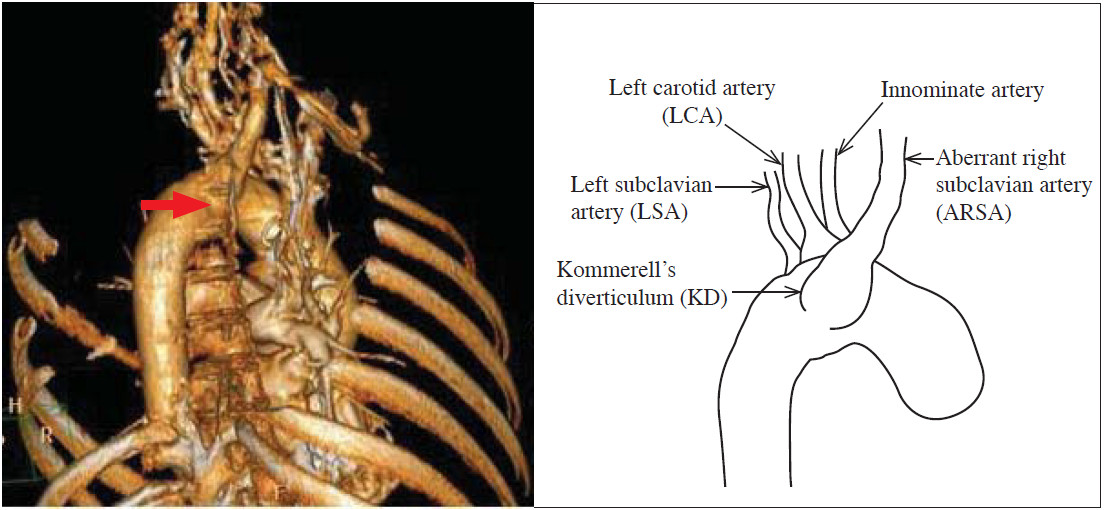
Figure 4: The 3D reconstruction computer tomography shows Kommerell’s diverticulum (KD), the back view (red arrow).
Aberrant right subclavian artery (ARSA) diverticulum is an extremely rare occurrence. Due to the extremely rare nature of the disease, the mortality and morbidity rates of its surgical treatment are still unclear. Some case reports on the surgical treatment of ARSA aneurysms have been published, but it is very difficult to ascertain the mortality and morbidity associated with this operation from these as it is likely that only successful cases have been published.
The first successful repair of an ARSA was reported by Gross.7 However, the best surgical approach to treat patients with pathologies of the lusorian artery is still a point of discussion. The division of the proximal part of the ARSA is the recommended surgical procedure in symptomatic patients. For patients with an aneurysm of ARSA or Kommerell’s diverticulum, exclusion is performed by the right or left thoracotomy, sternotomy, or transaortic repair with extracorporal circulation according to the underlying pathology and the site of the aortic arch. Kieffer and colleagues reported the largest single-center series with 33 patients treated for asymptomatic or aneurysmal of ARSA.8 According to their data, the perioperative mortality rate in the group of patients with aneurysmal disease of the ARSA was 23.5%. Nowadays, the endovascular surgery or combined surgical and endovascular treatment of patients with symptomatic pathologies of ARSA is an alternative treatment and used worldwide. Based on the reports in the literature, the combined endovascular occlusion of the aortic origin of the ARSA with subclavian artery transposition and distal prevertebral occlusion seems to be a safe and effective alternative for elective treatment, with no perioperative deaths so far. However, there is no report of long-term results.9-14
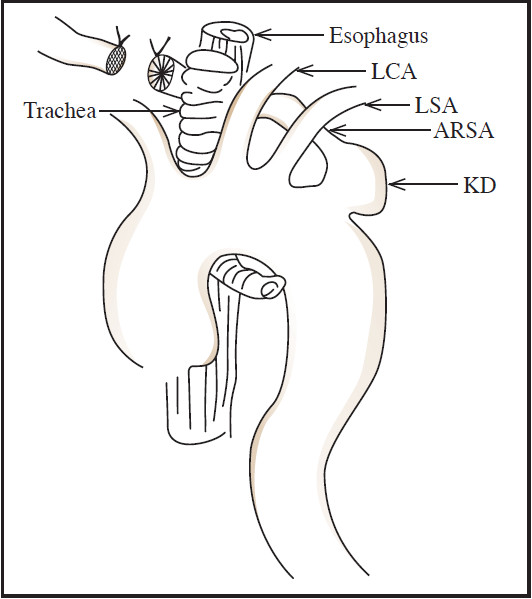
Figure 5: A drawing of the operative procedure for this patient.
Occlusion of the proximal ARSA without subclavian artery reconstruction might cause right arm ischemia or symptoms described as subclavian steal syndrome. The RSA transposition in cases of combined surgical and endovascular treatment for ARSA aneurysms are believed to be increasingly necessary to prevent reduction in cerebrobasilar blood flow. That said, the experience with the thoracic stent graft implantation in the proximal descending aorta with occlusion of the left subclavian artery (LSA) suggests sufficient blood supply to the left arm without transposition of the LSA.15
An ARSA can cause relevant symptoms due to compression of the esophagus or the trachea in association with or without an ARSA aneurysm. Operative repair by open surgery or in combination with an endovascular procedure is recommended to treat these symptoms and to reduce the risk of aneurysm rupture. Symptomatic patients can be treated by either a supraclavicular or transthoracic repair or an extrathoracic cervical-endovascular approach with a transbrachial proximal stent graft occlusion. Our experience suggests that a proximal descending aortic endovascular implantation without a left subclavian bypass causes no limb ischemia. The technique of dividing the ARSA without subclavian transposition which has been used in some cases produced no ischemic complications.
For patients with an ARSA aneurysm or an aneurysm of the proximal descending aorta, a thoracic aortic stent graft implantation to occlude the origin of the ARSA in combination with a distal occlusion of the ARSA and a subclavian artery transposition is the alternative treatment which is a minimally invasive approach with promising mid-term results. However, as there have only been a few cases of patients being treated with endovascular proce- dures so far, long-term results of a larger group of patients should be studied.
We report our successful surgical experience in a case of aberrant right subclavian artery (ARSA) aneurysm.